April 18, 2023
Auditorium, Room 2000 and 4th Floor
RCB/WVU HSC/Charleston Division
Agenda:
8:00 am – 5:30 pm
POSTER PRESENTATIONS
Oral Original Research and Oral Case Reports
Live and Streamed Event
http://camcinstitute.org/video/live
Poster Presentations –
- Research Day – POSTERS – Original Research -4th Floor/WVU - LIVE
Join Zoom Meeting - (save this link on your calendar/device)
https://zoom.us/j/4235949369?pwd=S0l6ZFZRaXU5ZGJJZ2tHKzB6NDc5UT09
- Research Day – POSTERS – Case Reports- Room 2000/WVU - LIVE
Join Zoom Meeting (save this link on your calendar/device)
Join Zoom Meeting
https://zoom.us/j/97553738065?pwd=K0pzbXZacVAySlJJdTgzWlExNWJaUT09
RESEARCH DAY:
Research Day was initiated in 1980 and was preceded by a similar event entitled Alumni-Education Day. This event has traditionally been planned to showcase research work completed by medical students, pharmacy students, nursing students and residents.
This year’s program continues to feature a collaborative effort of students and resident presentations with faculty/medical staff/professional staff preceptors. Research Day awards will be presented at the conclusion of this program for participants presenting student/resident research projects.
Objectives:
Upon completion of this program, attendees should be able to:
1) Describe ongoing research in the CAMC and WVU/Charleston medical community
2) Discuss case reports and their role in the practice of medicine
3) Encourage principal investigators/preceptors, residents, and students in their pursuits
in the area of clinical research
4) Express options for integrating new knowledge gained from research presentations into the clinical practice
Credit:
Physician and Nursing Participants may submit for self-claim credit at this event for attendance at any/all portions of the program at their discretion.
Thank you to the following:
Research Day Planning Committee: Steve Jubelirer, MD, (Honorary Chair); Amna Anees, MD, Javaria Anwar, MD, Scott Dean, PhD, Nancy Duvall, BSN, MS, RN-BC, Mary Emmett, PhD, Jade Gallimore, DO, Dan Lucas, PharmD, Elaine Davis, EdD, BSN, Robin Rector, MA and Michael Whitler.
CAMC IRB: Chris Terpening, PhD, PharmD (CHAIR); Atul Singh, DO, Deepay Mukerjee, MBA, Jennifer Gorrell, PharmD, Jessica Luzier, PhD, Melanie Whelan, PhD, Jessica Sop, DO, Christine Teague, PharmD, Hani Nazha, MD, Marciano B. Lee, MD, Rayan Ihle, MD, Sachin Bendre, MD, Sarah Rahman, MD, Samuel Deem, DO, Stephen Bush, MD, Zachary AbuRahma, DO, Heidi Edwards, MSN, Christina Thompson, MSN, Rev. Matt Friend, Michael Martin
CAMC ISRB: Scott Fields, PhD (CHAIR), Anjlee Patel, MD, MBA, James Campbell, MD, Karen Hannah, MBA, Mary Ann Maurer, DO, Patrick Kerr, PhD. Wesley Kafka, PharmD, Byron Calhoun, MD, James Harman, MD, Nathan Hale, DO, Tiffany Lasky, DO, Terrie Lee, MPH
A Special Thanks:
The Research Day Planning Committee has requested that a special thank you be shared with all preceptors, mentors, research associates, editors of abstracts, and reviewers of poster presentations that may have formally or informally assisted our learners with their research endeavors.
Poster Sessions – DUAL ZOOM INVITES
If you would like to hear a presentation on the named research – you should plan to attend the judging session for each poster noted below. Questions may only be asked by the judging panel.
Poster Session I:
8:20 am Poster #1 – Case
CASE REPORT: Mixed Germ Cell Tumor of the Ovary
Philip R. Fending, MD – Obstetrics and Gynecology
Preceptor: Stephen H. Bush, II
Poster A – Original
ORIGINAL: Follow Up Skeletal Surveys in Suspected Non-Accidental Trauma;
Yield and Examining Current Clinical Practice in Southern West Virginia
Umer Muhammad, MD – Pediatrics
Preceptor: Sharon Istfan, MD
8:30 am Poster #2 – Case
CASE REPORT: Scoping the Distance
Rebecca Spinaris, DO – Urological Surgery
Preceptor: Joshua Lohri, DO
Poster B – Original
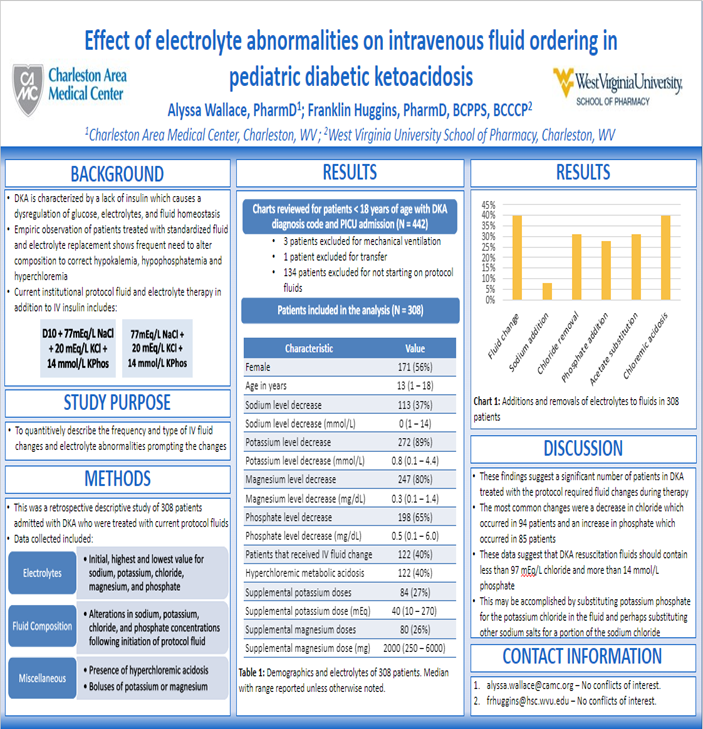
ORIGINAL: Effect of Electrolyte Abnormalities on Intravenous Fluid Ordering in
Pediatric Diabetic Ketoacidosis
Alyssa Wallace, PharmD - Pharmacy
Preceptor: Franklin Huggins, PharmD
8:40 am Poster #3 – Case
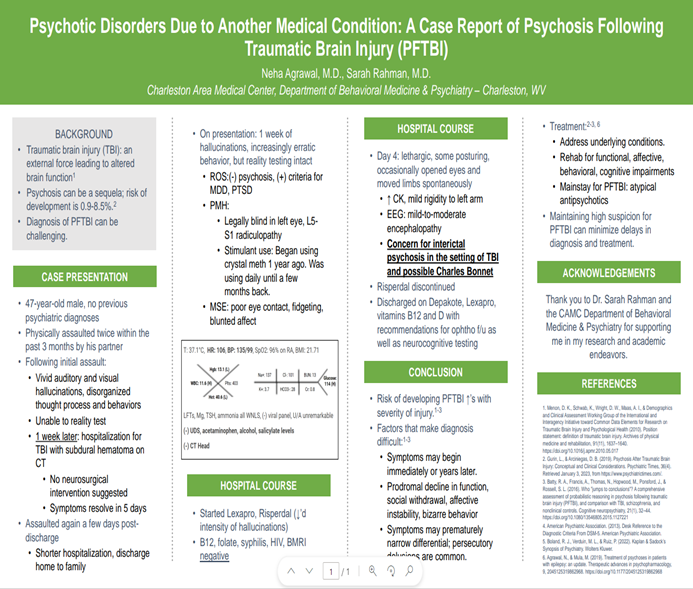
CASE REPORT: Psychotic Disorders Due to Another Medical Condition: A Case Report of
Psychosis Following Traumatic Brain Injury (PFTBI)
Neha Agrawal, MD – Internal Medicine/Psychiatry
Preceptor: Sarah Rahman, MD
Poster C – Original
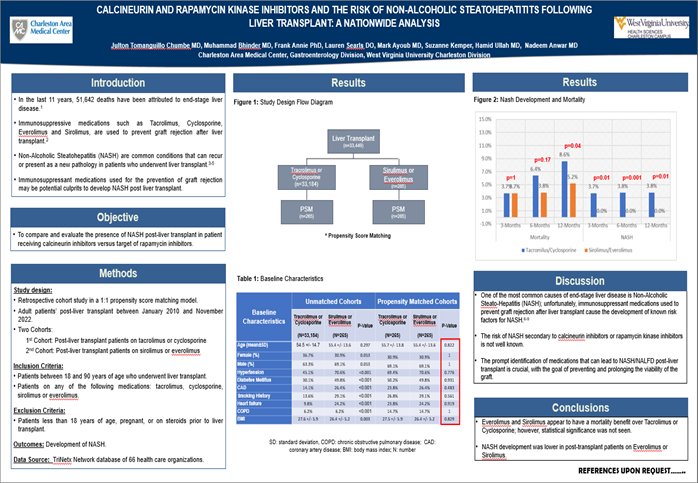
Original: Calcineurin and Rapamycin Kinase Inhibitors and The Risk of Non-alcoholic
Steatohepatitis Following Liver Transplant: A Nationwide Analysis
Muhammad Mujtaba Bhinder, MD, MBBS – Internal Medicine
Preceptor: Nadeem Anwar, MD
8:50 am Poster #4 – Case
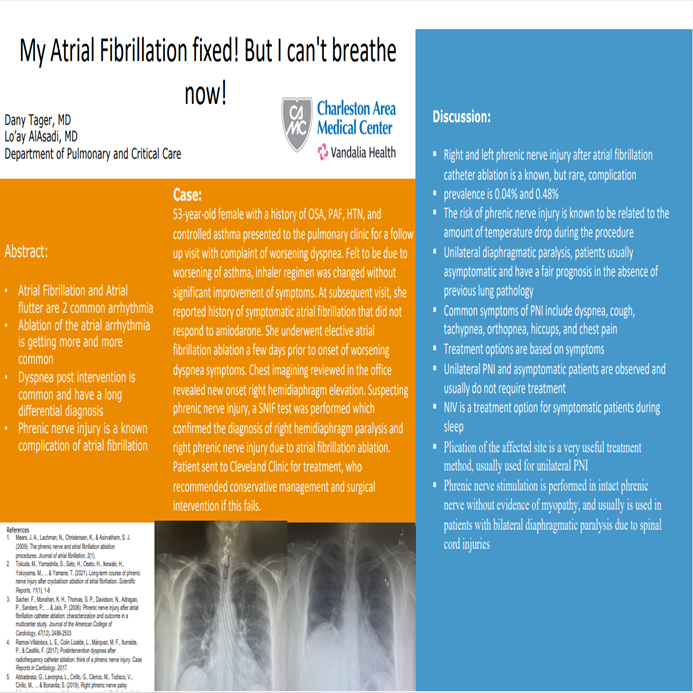
CASE REPORT: My Atrial Fibrillation Fixed! But I Can't Breath Now!
Dany Tager, MD – Pulmonary Critical Care
Preceptor: Lo’ay Al-Asadi, MD
Poster D – Original
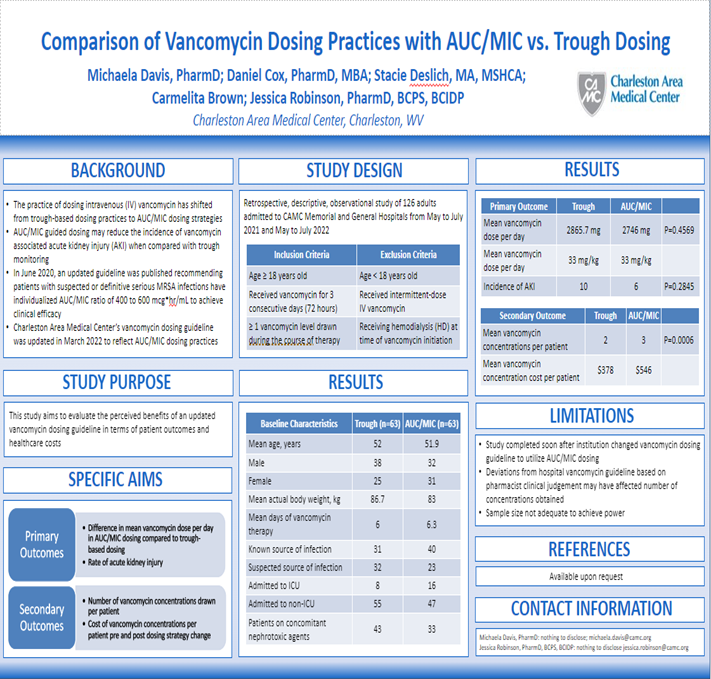
ORIGINAL: Comparison of Vancomycin Dosing Practices with AUC/MIC vs. Traditional Dosing
Michaela Davis, PharmD - Pharmacy
Preceptor: Jessica Robinson, PharmD
9:00 am Poster #5 – Case
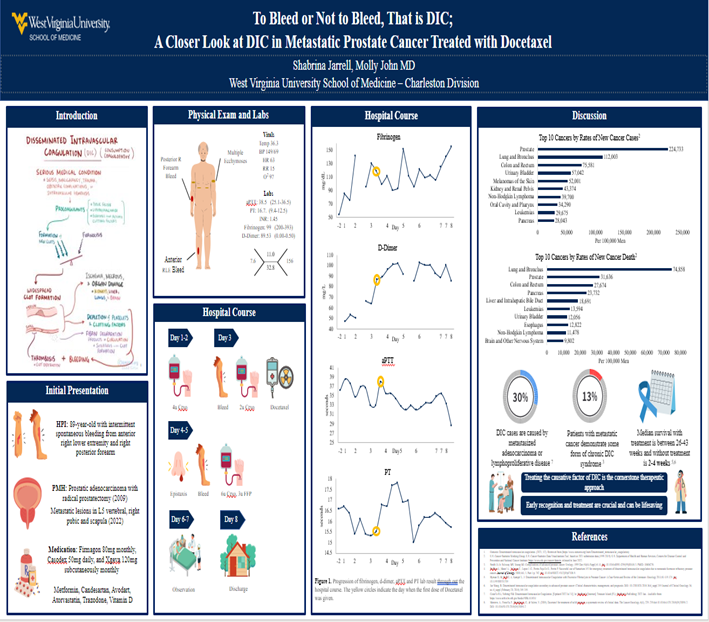
CASE REPORT: To Bleed or Not to Bleed, That is DIC; A Closer Look at DIC in Metastatic
Prostate Cancer Treated with Docetaxel
Shabrina Jarrell – Medical School - WVU
Preceptor: Molly John, MD
Poster E – Original
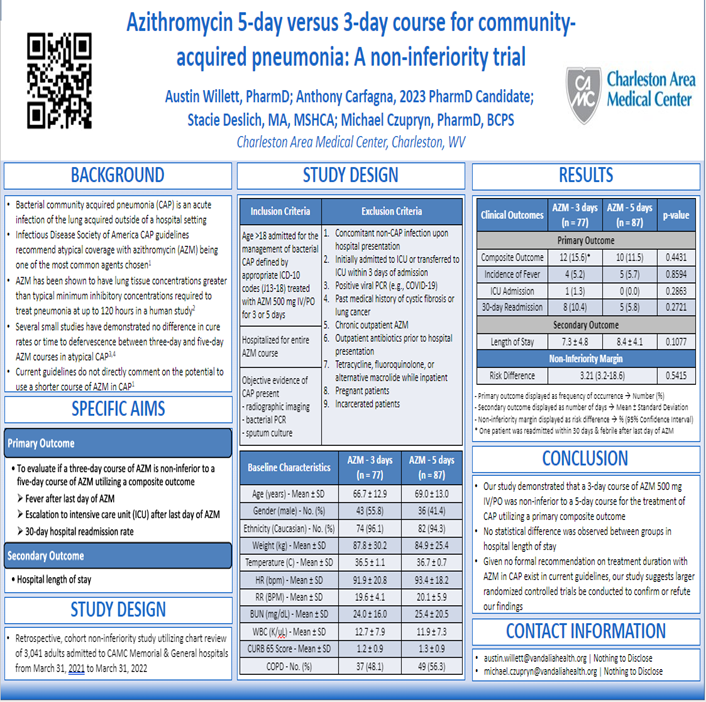
ORIGINAL: Azithromycin 5-day Versus 3-Day Course for Community Acquired Pneumonia: A Non-Inferiority Trial
Austin Willett, PharmD - Pharmacy
Preceptor: Michael Czupryn, PharmD
9:10 am Poster #6 – Case
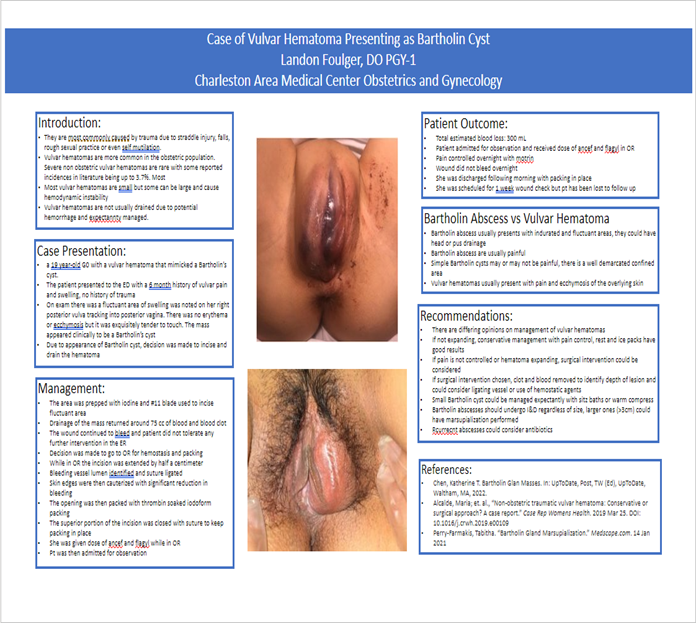
CASE REPORT: Vulvar Hematoma Presenting as Bartholin's Cyst
Landon Foulger, DO – Obstetrics and Gynecology
Preceptor: Karinna Andrews, DO
Poster F – Original
ORIGINAL: A Nationwide Analysis of The Impact of Direct Oral Anticoagulants In Patients With Compensated Cirrhosis and Portal Vein Thrombosis
Mark Ayoub, MD – Internal Medicine
Preceptor: Nadeem Anwar, MD
9:20 am Poster #7 – Case
CASE REPORT: CLOVES Syndrome
Brittany Crabtree, MD – Obstetrics and Gynecology
Preceptor: Byron Calhoun, MD
Poster G – Original
ORIGINAL: Evaluation of Overcorrection of Hyponatremia in the Intensive Care Unit
Rachel Cruickshank, PharmD - Pharmacy
Preceptor: Jennifer Chaffin, PharmD
9:30 am Judges Break
Poster Session II
9:50 am Poster #8– Case
CASE REPORT: SVC Syndrome
Anna Wang – Medical Student – WVU
Preceptor: Courtney Beasley, DO
Poster H – Original
ORIGINAL: Depression and Perioperative Chemotherapy in Bladder Cancer Patients
Matthew DeSanto, MD – Urological Surgery
Preceptor: Nathan Hale, DO
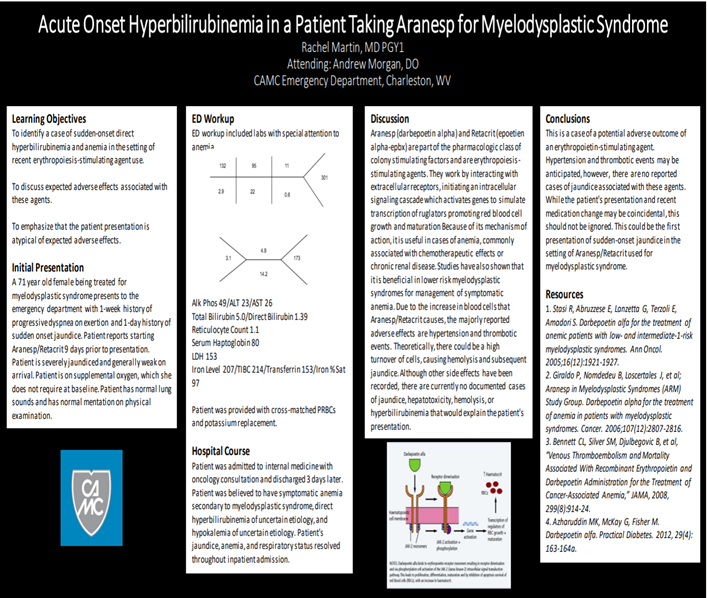
10:00 am Poster #9- Case
CASE REPORT: Acute Onset Hyperbilirubinemia in a Patient Taking Aranesp for
Myelodysplastic Syndrome
Rachel Martin, DO – Emergency Medicine
Preceptor: Andrew Morgan, DO
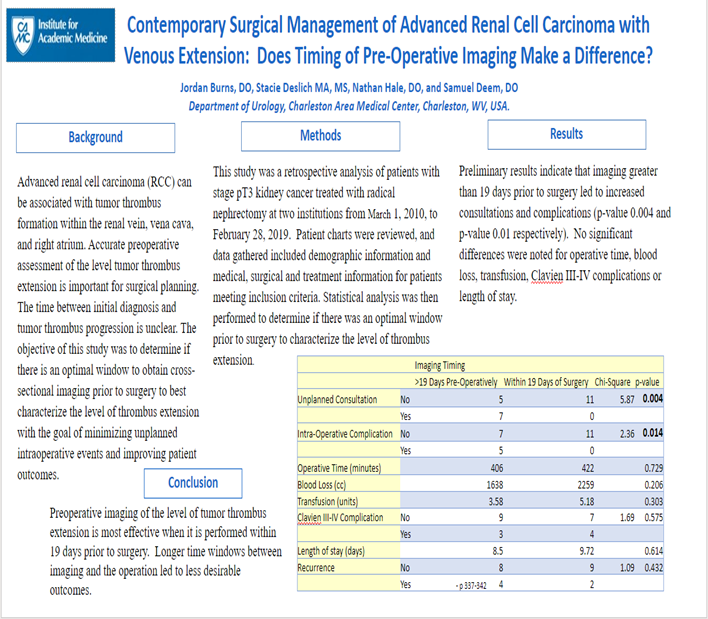
Poster I – Original
ORIGINAL: Contemporary Surgical Management of Advanced Renal Cell Carcinoma with
Venous Extension: Does Timing of Pre-operative Imaging Make a Difference?
Jordon Burns, DO – Urological Surgery
Preceptor: Nathan Hale, DO
10:10 am Poster #10 – Case
CASE REPORT: Mutating Muscles: Pediatric Solitary Papillary Muscle Hypertrophy
as a Variant of Hypertrophic Cardiomyopathy
Rojin Arefi, MD – Pediatrics
Preceptor: Anjlee Patel, MD
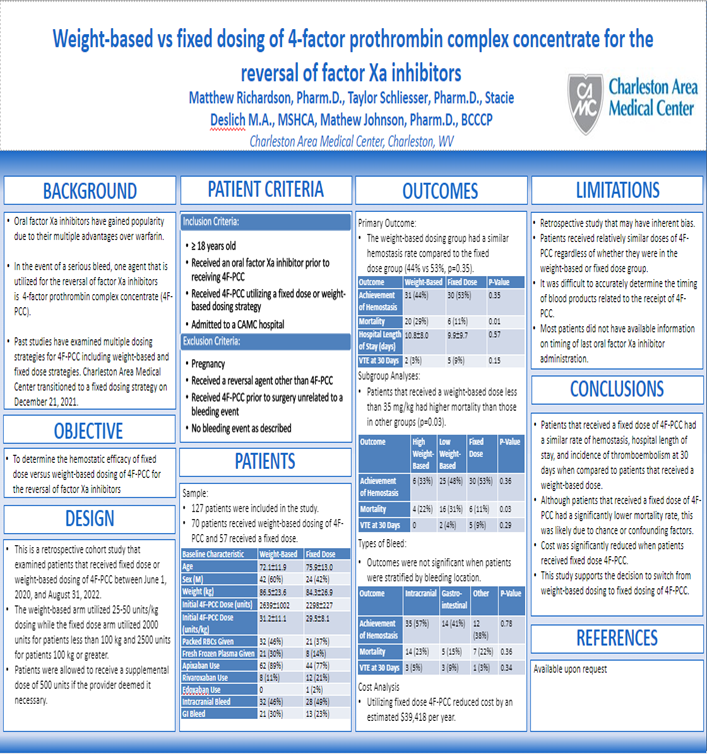
Poster J – Original
ORGINAL: Fixed Dose 4-Factor Prothrombin Complex Concentrate for the Reversal of
Factor Xa Inhibitors
Matthew Richardson, PharmD - Pharmacy
Preceptor: Mathew Johnson, PharmD
10:20 am Poster #11 – Case
CASE REPORT: LCV Inflammation
Joseph Del Zotto, DO – Emergency Medicine
Preceptor: Amy Hunt, DO
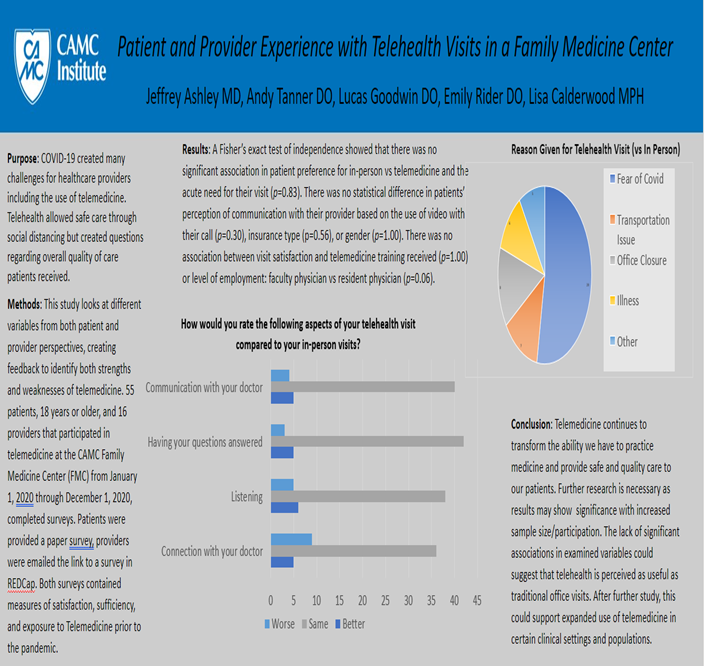
Poster K – Original
ORIGINAL: Patient and Provider Experience with Telehealth Visits in a Family Medicine Center
Lucas Goodwin, DO – Family Medicine
Preceptor: Andy Tanner, DO
10:30 am Poster #12 – Case
CASE REPORT: Acute Valproic Acid Toxicity After Intentional Overdose
Joseph Blumer, DO – Emergency Medicine
Preceptor: Brian Hensley, MD
Poster L – Original
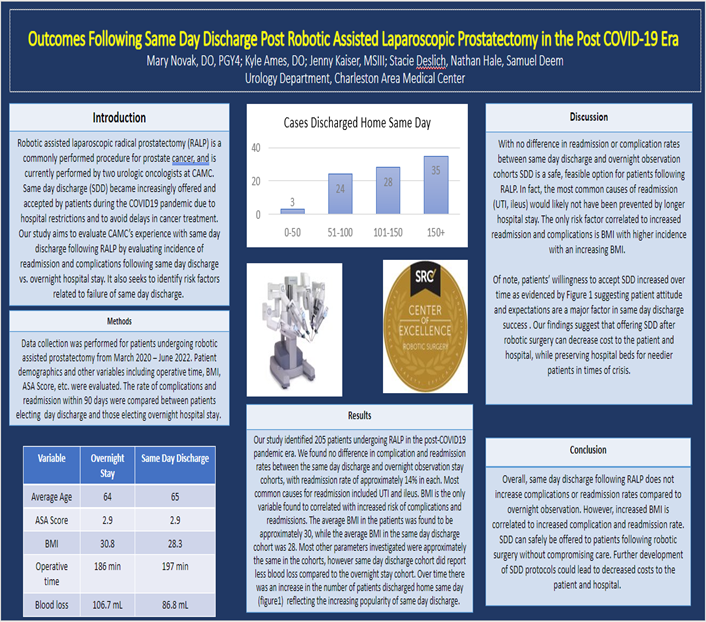
ORIGINAL: Outcomes Following Same Day Discharge Post-RALP in the Post-COVID19 Era
Mary Novak, DO
Preceptor: Samuel Deem, DO
10:40 am Poster #13 – Case
CASE REPORT: A Case of Synovial Sarcoma of the Vulva
Jessica Allen, MD – Obstetrics and Gynecology
Preceptor: Stephen H. Bush, II, MD
Poster M – Original
ORIGINAL: Medication-Related Fall Risk Among Anticoagulated Older Adults Evaluated for a Fall Injury in an Emergency Department: identification and Communication During the Transitions of Care
Justi Mueller, PharmD - Pharmacy
Preceptor: David Elliott, PharmD
10:50 am Poster #14 – Case
CASE REPORT: A Rare Case of Pulmonary Mucormycosis in an Immunocompetent Patient
Syed Kashif Mahmood, MD – Pulmonary & Critical Care
Preceptor: Loay Al-Asadi, MD
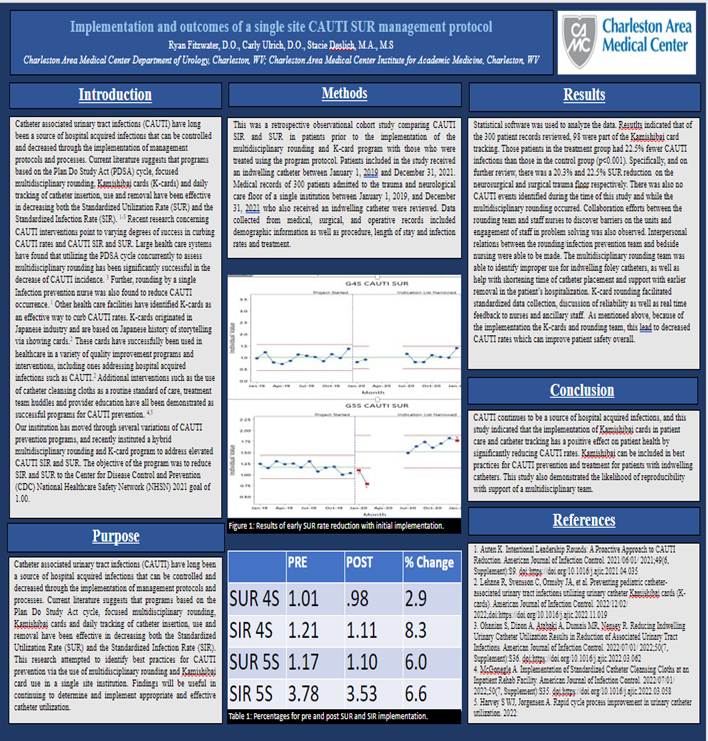
Poster N – Original
Implementation and Outcomes of a Single-Site CAUTI SUR Management Protocol
Carly Ulrich, DO
Preceptor: Ryan Fitzwater, DO
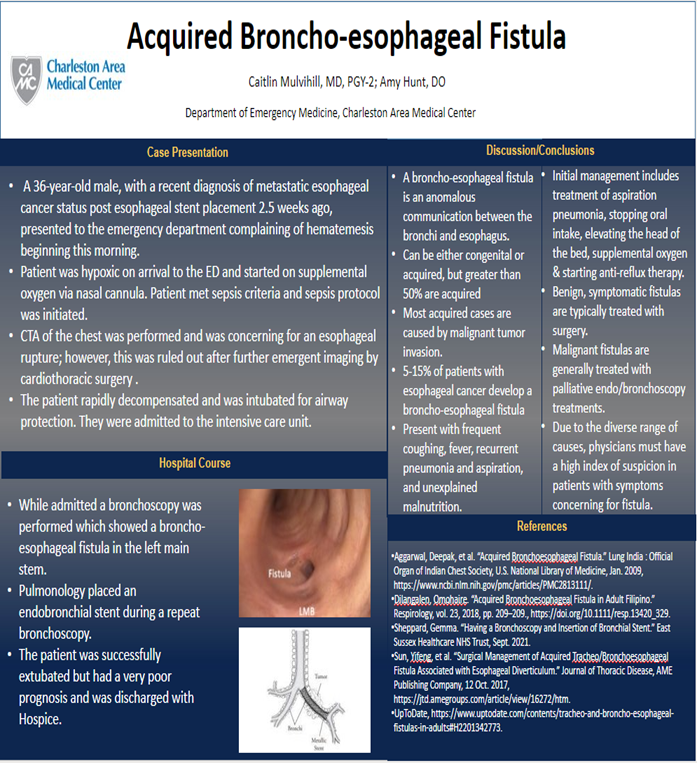
11:00 am Poster #15 - Case
CASE REPORT: Acquired Bronchoesophageal Fistula
Caitlin Mulvihill, MD – Emergency Medicine
Preceptor: Amy Hunt, DO
11:10 am Poster #16 – Case
CASE REPORT: Opsoclonus Myoclonus Syndrome in Pregnancy
Erin Light, MD – Obstetrics and Gynecology
Preceptor: Byron Calhoun, MD
11:20 am Poster #17 – Case
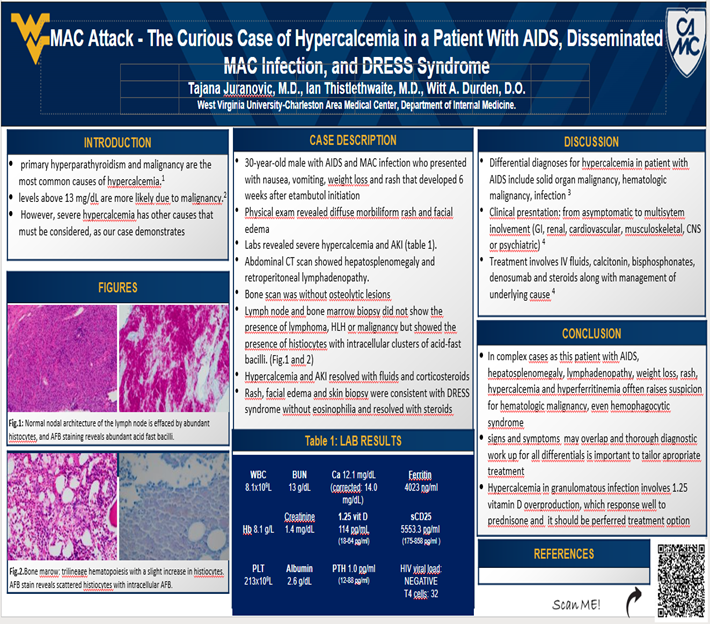
CASE REPORT: MAC Attack - The Curious Case of Hypercalcemia in a Patient With AIDS, Disseminated MAC Infection, and DRESS Syndrome
Tajana Juranovic, MD – Internal Medicine
Preceptor: A. Durden Witt, DO
11:30 am Poster #18 – Case
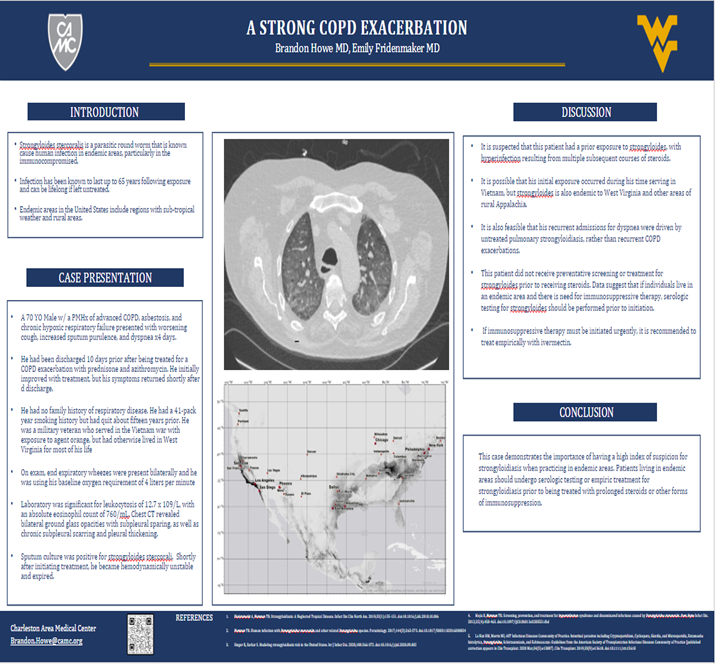
CASE REPORT: A Strong COPD Exacerbation
Brandon Howe, MD – Internal Medicine
Preceptor: Emily Fridenmaker, MD
11:40 am Poster #19 – Case
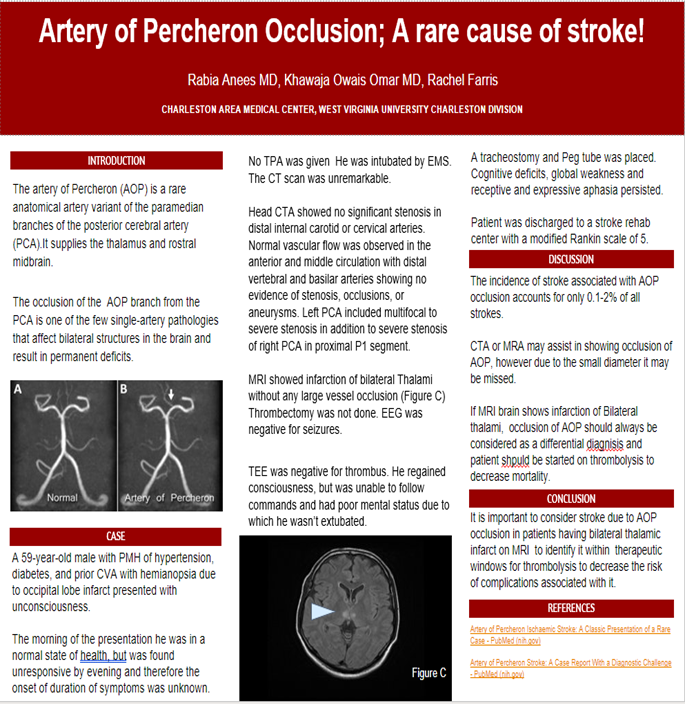
CASE REPORT: Artery of Percheron Occlusion; A Rare Cause of Stroke!
Rabia Anees, MD – Internal Medicine
Preceptor: Khawaja Owais Omar, MD
11:50 am Poster #20 – Case
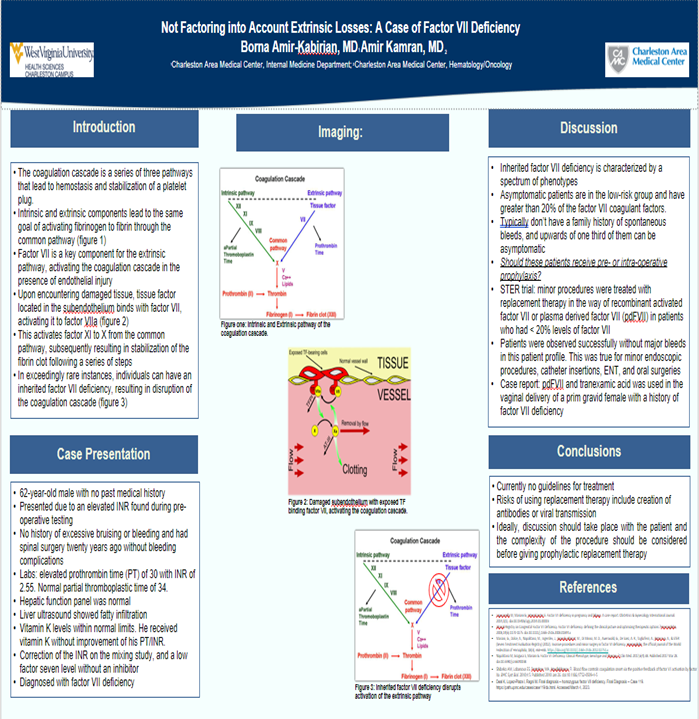
CASE REPORT: Not Factoring into Account Intrinsic Losses- A Case of Factor VII Deficiency
Borna Amir-Kabirian, MD – Internal Medicine
Preceptor: Amir Kamran, MD
12:00 noon Lunch - Judges Break
Poster Session III
1:00 pm Poster #21 – Case
CASE REPORT: A Grave Matter Post Covid Infection
Parisa Aijaz, MD – Internal Medicine
Preceptor: Amna Anees, MD
1:10 pm Poster #22 – Case
CASE REPORT: Subxiphoid Pericardial Fluid Collection after Pericardial Window,
Chest Compressions, and Severe Cough
Chloe Kellum – Medical Student - WVU
Preceptor: Shawn Chillag, MD
1:20 pm Poster #23 – Case
CASE REPORT: Danger Gummies: Δ8 -THC Induced Psychosis, A Case Series
Manisha Kukkillaya - Medical Student - WVU
Preceptor: James Griffith, MD
1:30 pm Poster #24– Case
CASE REPORT: All About That Base
Jarrod Kahre, DO – Emergency Medicine
Preceptor: Joshua Burg, DO
1:40 pm Poster #25 – Case
CASE REPORT: Why Can’t I Breathe? Dapsone Induced Methemoglobinemia in Child with Leukemia
Adam Whiteley, MD - Pediatrics
Preceptor: Sana Farooki, MD
1:50 pm Poster #26 – Case
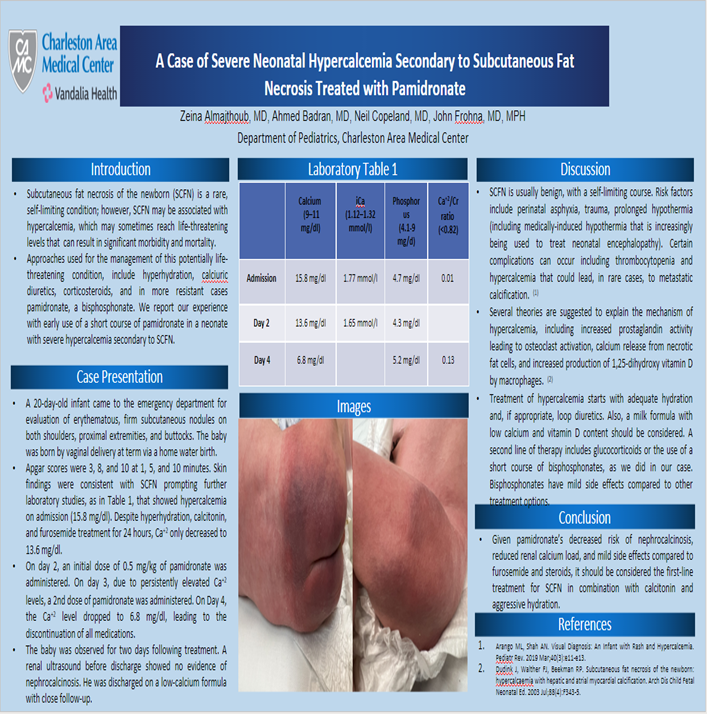
CASE REPORT: A Case of Severe Neonatal Hypercalcemia Secondary to Subcutaneous
Fat Necrosis Treated with Pamidronate
Zeina Almajthoub, MD- Pediatrics
Preceptor: John Frohna, MD
8:20 am Poster #1 – Case
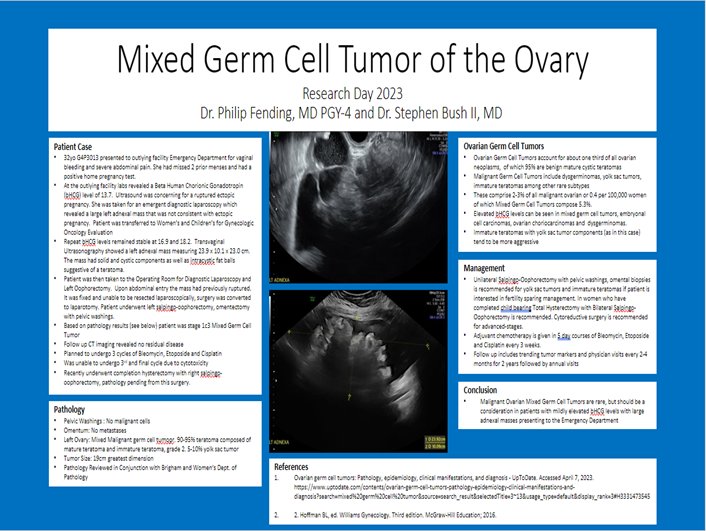
CASE REPORT: Mixed Germ Cell Tumor of the Ovary
Philip R. Fending, MD – Obstetrics and Gynecology
Preceptor: Stephen H. Bush, II
Mixed Germ Cell Tumors are a rare cause of ovarian malignancy. They comprise of less than 5% of all ovarian neoplasms in adult females. The patient is a 32yo G4P3013 presenting to an outlying facility with complaints of severe abdominal pain with associated vaginal spotting. Patient had taken multiple home pregnancy tests which were positive and she had planned to follow up with her gynecologist as an outpatient. On presentation the patient was found to have a quantitative human chorionic gonadotropin (HCG) level of 13.7. Ultrasound revealed large volume free fluid and the patient was taken for emergent diagnostic laparoscopy for suspected ruptured ectopic pregnancy. Upon entry a large left sided ovarian mass was encountered estimated to be approximately 20cm in diameter. The patient was then transferred to CAMC under Gynecologic Oncology for further workup of the large ovarian mass. Her HCG remained elevated at 16.9 and 18.2. Ultrasound completed at our facility revealed a 23.9 x 10.1 x 23.0 cm left adnexa with a solid mass containing cystic components and intracystic fat globules, potentially consistent with teratoma. Due to the size of the mass, we recommended diagnostic laparoscopy with left salpingo-oophorectomy for pathologic evaluation of the mass. Upon laparoscopic entry it became evident that the case could not be completed with minimally invasive technique and we converted to open left salpingo-oophorectomy and omentectomy. Patient did well postoperatively. Her HCG level trended down to 9.7 and 4.4 on postoperative days 1 and 2 respectively. She was discharged home on postoperative day 2. Final pathology was significant for mixed malignant germ cell tumor composed of 90-95% teratoma with both mature and immature components and 5-10% yolk sac tumor. The patient is currently undergoing chemotherapy with bleomycin, etoposide and cisplatin.
8:20 am Poster #1 – Case
CASE REPORT: Mixed Germ Cell Tumor of the Ovary
Philip R. Fending, MD – Obstetrics and Gynecology
Preceptor: Stephen H. Bush, II
8:20 am Poster A – Original
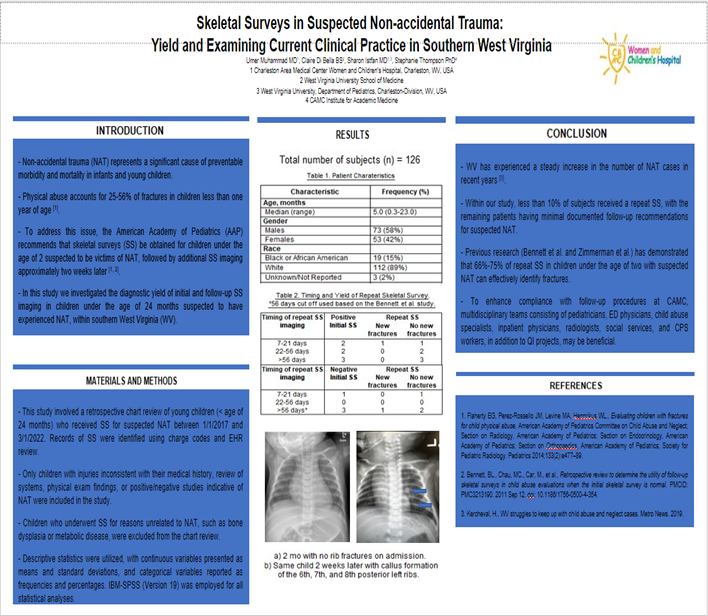
ORIGINAL: Follow Up Skeletal Surveys in Suspected Non-Accidental Trauma;
Yield and Examining Current Clinical Practice in Southern West Virginia
Umer Muhammad, MD – Pediatrics
Preceptor: Sharon Istfan, MD
Introduction: Child abuse has been on the rise and is frequently encountered by pediatricians and child advocacy specialists all over the United States. The number of suspected and confirmed non-accidental trauma (NAT) cases has steadily risen over the past few years in West Virginia. When child abuse is suspected, the American Academy of Pediatrics (AAP) recommends evaluating children <2 years of age with initial skeletal surveys (series of bone X-rays; SS) to identify acute, healing, or old fractures and to repeat the SS 11-14 days after the initial survey, as bone calcification and bone healing indicative of fracture may be delayed. However, due to various reasons such as radiation exposure, medical/financial burdens, and inconvenience to the families, many children do not receive repeat imaging.
Methods: We reviewed charts of 126 children under the age of 2 years who received SS due to physical abuse suspicion at our hospital between 1/1/2017 and 03/1/2022.
Results: A total of 61 (48%) initial SS showed fractures. Results from our study found that repeat SS, done in cases where the initial SS was positive, can continue to show signs of healing up to 16 days after initial imaging. On the other hand, repeat SS done for initial negative scans, continued to be negative except for in one case when it was positive >6months. Lastly, only 48% of patients received consults from child abuse specialists in our study.
Conclusion: Repeating SS in cases of initial negative is valuable as they help with identifying fractures that may not be detectable on initial scans, like rib fractures. Furthermore, consulting child abuse specialists should not be overlooked irrespective of positive or negative initial SS findings as these professionals are trained in the art of providing specialized care for children who are victims of NAT.
8:20 am Poster A – Original
ORIGINAL: Follow Up Skeletal Surveys in Suspected Non-Accidental Trauma;
Yield and Examining Current Clinical Practice in Southern West Virginia
Umer Muhammad, MD – Pediatrics
Preceptor: Sharon Istfan, MD
8:30 am Poster #2 – Case
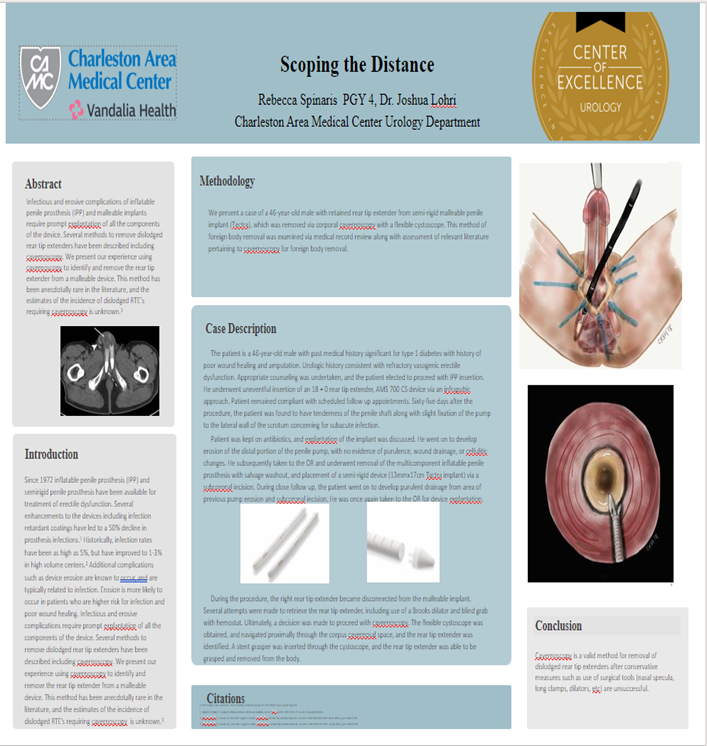
CASE REPORT: Scoping the Distance
Rebecca Spinaris, DO – Urological Surgery
Preceptor: Joshua Lohri, DO
Purpose: Infectious and erosive complications of inflatable penile prosthesis (IPP) and malleable implants require prompt explantation of all the components of the device. Several methods to remove dislodged rear tip extenders have been described including cavernoscopy. We present our experience using cavernoscopy to identify and remove the rear tip extender from a malleable device. This method has been anecdotally rare in the literature, and the estimates of the incidence of dislodged RTE’s requiring cavernoscopy is unknown.3
Methods: Case of a 46-year-old male with retained rear tip extender from semi-rigid malleable penile implant, which was removed via cavernoscopy. This method of foreign body removal was examined via medical record review along with assessment of relevant literature pertaining to cavernoscopy for foreign body removal.
Case Description: The patient is a 46-year-old male with past medical history significant for type 1 diabetes with history of poor wound healing and amputation. Urologic history consistent with refractory vasogenic erectile dysfunction. Appropriate counseling was undertaken, and the patient elected to proceed with IPP insertion. He underwent uneventful insertion of an 18 + 0 rear tip extender, AMS 700 CS device via an infrapubic approach. Patient remained compliant with scheduled follow up appointments. Sixty-five days after the procedure, the patient was found to have tenderness of the penile shaft along with slight fixation of the pump to the lateral wall of the scrotum concerning for subacute infection. Patient was kept on antibiotics, and explantation of the implant was discussed. He went on to develop erosion of the distal portion of the penile pump, with no evidence of purulence, wound drainage, or cellulitic changes. He subsequently taken to the OR and underwent removal of the multicomponent inflatable penile prosthesis with salvage washout, and placement of a semi-rigid device (13mmx17cm Tactra implant) via a subcoronal incision. During close follow up, the patient was found to have purulent drainage from the incision site. He was once again taken to the OR for device explantation. During the procedure, the right rear tip extender became disconnected from the malleable implant. Several attempts were made to retrieve the rear tip extender, including use of a Brooks dilator and blind grab with hemostat. Ultimately, a decision was made to proceed with cavernoscopy. The flexible cystoscope was obtained, and navigated proximally through the corpus cavernosal space, and the rear tip extender was identified and removed.
Conclusion: Cavernoscopy is a valid method for removal of dislodged rear tip extenders after conservative measures such as use of surgical tools (nasal specula, long clamps, dilators, etc) are unsuccessful.
8:30 am Poster #2 – Case
CASE REPORT: Scoping the Distance
Rebecca Spinaris, DO – Urological Surgery
Preceptor: Joshua Lohri, DO
8:30 am Poster B – Original
ORIGINAL: Effect of Electrolyte Abnormalities on Intravenous Fluid Ordering in
Pediatric Diabetic Ketoacidosis
Alyssa Wallace, PharmD - Pharmacy
Preceptor: Franklin Huggins, PharmD
OBJECTIVE
Empiric observation of patients treated with a standardized fluid and electrolyte replacement protocol shows frequent need to alter composition of IV fluids to correct hypokalemia, hypophosphatemia and hyperchloremia. We hypothesize that quantitively describing the frequency and nature of IV fluid changes and electrolyte abnormalities that prompt those changes may inform the design of empiric fluids. This could minimize the frequency of electrolyte abnormalities and fluid changes during DKA therapy.
METHODS
This was a retrospective descriptive study of patients admitted to the pediatric ICU with a diagnosis of DKA between September 2016 and December 2021 who were treated with current institutional protocol fluids. If a patient was started on the institutional fluid protocol, their initial, lowest, and highest serum values for sodium, potassium, chloride, magnesium, and phosphate were recorded. These patients were then examined to see whether these fluctuations resulted in IV fluid alterations or electrolyte supplementation.
RESULTS
There were 308 children included in the analysis. Of the patients that received the protocol fluids initially, 40% had changes made to their IV fluids. In patients included in the analysis, 40% developed hyperchloremic metabolic acidosis. The most common changes in fluids were a decrease in chloride (31%) and an increase in phosphate (28%).
CONCLUSIONS
Based on the results of this study, a significant number of patients in DKA treated with the protocol fluids required fluid changes during therapy. These data suggest that DKA resuscitation fluids should contain less than 97 mEq/L chloride and more than 14 mmol/L phosphate.
8:30 am Poster B – Original
ORIGINAL: Effect of Electrolyte Abnormalities on Intravenous Fluid Ordering in
Pediatric Diabetic Ketoacidosis
Alyssa Wallace, PharmD - Pharmacy
Preceptor: Franklin Huggins, PharmD
8:40 am Poster #3 – Case
CASE REPORT: Psychotic Disorders Due to Another Medical Condition: A Case Report of
Psychosis Following Traumatic Brain Injury (PFTBI)
Neha Agrawal, MD – Internal Medicine/Psychiatry
Preceptor: Sarah Rahman, MD
Introduction:
Traumatic brain injury (TBI) is defined as an external force leading to altered brain function.1 Psychosis can be a sequela of TBI; risk of development ranges from 0.9-8.5%. Diagnosing PFTBI is challenging.2 We present a case of a patient who experienced auditory hallucinations (AH), visual hallucinations (VH), and erratic behavior following TBI.
Case Presentation:
A 47-year-old male with no previous psychiatric diagnoses presented to the ED following 2 counts of physical assault by his partner within the past 3 months. Following the initial assault, he began experiencing vivid AH and VH, disorganized thoughts and behaviors. One week later, hospitalization at an outlying facility revealed a subdural hematoma without need for neurosurgical intervention; his symptoms of psychosis resolved within 5 days of hospitalization. He was assaulted again a few days post-discharge, followed by a shorter hospitalization and discharge home to family. One week prior to presentation in our ED, he again began experiencing AH, VH and disorganized behavior.
Treatment with Risperdal was initiated, and his hallucinations decreased in intensity. On day 4, he was found lethargic with elevated CK and EEG showing mild-to-moderate encephalopathy, suggesting interictal psychosis in the setting of TBI. Risperdal was discontinued; he was discharged on Depakote, Lexapro, and vitamins B12 and D with recommendations for neurocognitive testing.
Conclusion:
The risk of developing PFTBI increases with severity of injury, however, multiple factors can make it difficult to diagnose. Patients may experience symptoms immediately post-TBI or years later. They can exhibit prodromal decline in function, social withdrawal, affective instability, and bizarre behavior, as in our case. These symptoms may suggest a primary mood or psychotic disorder, prematurely narrowing the differential. Additionally, patients commonly present with persecutory delusions, whereas our patient predominantly exhibited hallucinations and disorganized behavior. Maintaining high suspicion for PFTBI can minimize delays in diagnosis and treatment.1-3
8:40 am Poster #3 – Case
CASE REPORT: Psychotic Disorders Due to Another Medical Condition: A Case Report of
Psychosis Following Traumatic Brain Injury (PFTBI)
Neha Agrawal, MD – Internal Medicine/Psychiatry
Preceptor: Sarah Rahman, MD
8:40 am Title: Poster C – Original
Original: Calcineurin and Rapamycin Kinase Inhibitors And The Risk Of Non-alcoholic
Steatohepatitis Following Liver Transplant: A Nationwide Analysis
Muhammad Mujtaba Bhinder, MD, MBBS – Internal Medicine
Preceptor: Nadeem Anwar, MD
Introduction: End-stage liver disease (ESLD) is a leading cause of mortality worldwide, with Non-Alcoholic Steatohepatitis (NASH) as one of the most common causes. Definitive treatment with liver transplant requires immunosuppressive agents to prevent graft rejection. These agents can cause the development of known risk factors for NASH like hypertension and diabetes; however, little is known of the risk for the development of NASH secondary to calcineurin inhibitors or mTOR kinase inhibitors. The objective of our study is to assess the risk of NASH development among patients on immunosuppressive treatment.
Method: This is a retrospective cohort study utilizing TriNetX, where post-liver transplant patients were identified between January 01, 2020, and November 1st, 2022, with 33,449 cases. Cohort 1 comprised post-liver transplant patients on Calcineurin Inhibitors (Tacrolimus or Cyclosporine), and cohort 2 comprised post-liver transplant patients on (mTOR Everolimus or Sirolimus). We created a propensity score matching of a 1:1 was performed to match on the covariates: Age, Gender, Hypertension, Diabetes, Heart Failure, CAD, COPD, History of smoking, and BMI. The endpoints of mortality (at 3-, 6- and 12-month’ intervals) and incidence of NASH were analyzed.
Results: A total of 33,449 patients were included. Liver transplant recipients on tacrolimus or cyclosporine were compared to those on Everolimus or Sirolimus. Mortality at 3 months was equal (3.7% vs 3.7%, P=1.00) in both groups, however, mortality was lower in the Everolimus or Sirolimus group at 6 months (3.77% vs 6.4%, P=0.17) and 1 year (5.2% vs 8.6%, P=0.04). NASH development was lower in the Everolimus and Sirolimus group at 3 months (0% vs 3.7, P=0.01), 6 months (0% vs 3.77, P=0.001), and 1 year (0% vs 3.7, P=0.01).
Conclusion: Everolimus and Sirolimus appear to have a mortality benefit over Tacrolimus or Cyclosporine, however, statistical significance was not seen. NASH development was lower in post-transplant patients on Everolimus or Sirolimus.
Authors: Bhinder, Muhammed; Tomanguillo Chumbe, Julton; Annie, Frank; Searls, Lauren; Ayoub, Mark; Kemper, Suzanne; Ullah, Hamid; Iqbal, Sara; Anwar, Nadeem
IRB #: 008363
8:40 am Title: Poster C – Original
Original: Calcineurin and Rapamycin Kinase Inhibitors And The Risk Of Non-alcoholic
Steatohepatitis Following Liver Transplant: A Nationwide Analysis
Muhammad Mujtaba Bhinder, MD, MBBS – Internal Medicine
Preceptor: Nadeem Anwar, MD
8:50 am Poster #4 – Case
CASE REPORT: My Atrial Fibrillation Fixed! But I Can't Breath Now!
Dany Tager, MD – Pulmonary Critical Care
Preceptor: Lo’ay Al-Asadi, MD
Case
53-year-old female with a history of OSA, PAF, HTN, and controlled asthma presented to the pulmonary clinic for a follow up visit with complaint of worsening dyspnea. Felt to be due to worsening of asthma, inhaler regimen was changed without significant improvement of symptoms. At subsequent visit, she reported history of symptomatic atrial fibrillation that did not respond to amiodarone. She underwent elective atrial fibrillation ablation a few days prior to onset of worsening dyspnea symptoms. Chest imagining reviewed in the office revealed new onset right hemidiaphragm elevation. Suspecting phrenic nerve injury, a SNIF test was performed which confirmed the diagnosis of right hemidiaphragm paralysis and right phrenic nerve injury due to atrial fibrillation ablation. Patient sent to Cleveland Clinic for treatment, who recommended conservative management and surgical intervention if this fails.
Discussion
Right and left phrenic nerve injury after atrial fibrillation catheter ablation is a known, but rare, complication. The prevalence is currently documented between 0.04% and 0.48%. Right phrenic nerve injury typically occurs after an ablation that is performed through pulmonary veins or the superior vena cava. Left phrenic nerve injury occurs when the ablation is performed through the left atrial appendage. The risk of phrenic nerve injury is known to be related to the amount of temperature drop during the procedure.
Unilateral diaphragmatic paralysis, patients usually asymptomatic and have a fair prognosis in the absence of previous lung pathology. Common symptoms of PNI include dyspnea, cough, tachypnea, orthopnea, hiccups, and chest pain.
Treatment options are based on symptoms. Unilateral PNI and asymptomatic patients are observed and usually do not require treatment. NIV is a treatment option for symptomatic patients during sleep. Plication of the affected site is a very useful treatment method, usually used for unilateral PNI. Phrenic nerve stimulation is performed in intact phrenic nerve without evidence of myopathy, and usually is used in patients with bilateral diaphragmatic paralysis due to spinal cord injuries.
8:50 am Poster #4 – Case
CASE REPORT: My Atrial Fibrillation Fixed! But I Can't Breath Now!
Dany Tager, MD – Pulmonary Critical Care
Preceptor: Lo’ay Al-Asadi, MD
8:50 am Poster D – Original
ORIGINAL: Comparison of Vancomycin Dosing Practices with AUC/MIC vs. Traditional Dosing
Michaela Davis, PharmD - Pharmacy
Preceptor: Jessica Robinson, PharmD
Purpose: In recent years, the practice of dosing intravenous vancomycin has shifted from trough-based dosing practices to AUC/MIC dosing strategies. In 2022, Charleston Area Medical Center (CAMC) adopted an AUC/MIC vancomycin dosing guideline after previously dosing based on a trough concentration protocol. This study aims to evaluate the perceived benefits of an updated vancomycin dosing protocol in terms of patient outcomes and healthcare costs.
Methods: This is a retrospective descriptive, observational study of adult patients admitted to CAMC Memorial and General Divisions who received intravenous vancomycin during their admission. The study examines patients monitored by trough-based dosing from May to July 2021 and patients monitored by AUC/MIC dosing from May to July 2022. Patients were identified from an internal report of Pharmacy-to-Dose vancomycin consults and evaluated for pre-defined inclusion and exclusion criteria. Comparisons were drawn from intravenous vancomycin exposure per day for patients being monitored with AUC/MIC guideline implementation versus traditional trough monitoring.
Results: Our initial analysis indicates that patients within the AUC/MIC group are receiving similar doses of vancomycin when compared to those in the trough monitoring group (2746 mg vs 2865 mg, P=0.4569) and fewer patients are meeting the KDIGO definition of acute kidney injury (6 vs 10 patients). More concentrations were obtained for patients within the AUC/MIC group as compared to patients who received trough-based dosing.
Conclusions: Change in dosing protocol from trough-based to AUC/MIC dosing resulted in similar vancomycin doses and increased number of concentrations per patient. The total number of vancomycin concentrations is dependent mainly upon vancomycin duration of treatment. This study provides baseline information regarding the usage of vancomycin after changing the dosing protocol.
8:50 am Poster D – Original
ORIGINAL: Comparison of Vancomycin Dosing Practices with AUC/MIC vs. Traditional Dosing
Michaela Davis, PharmD - Pharmacy
Preceptor: Jessica Robinson, PharmD
9:00 am Poster #5 – Case
CASE REPORT: To Bleed or Not to Bleed, That is DIC; A Closer Look at DIC in Metastatic
Prostate Cancer Treated with Docetaxel
Shabrina Jarrell – Medical School - WVU
Preceptor: Molly John, MD
As the second leading cause of cancer death in American men, prostate cancer can progress to many disabling symptoms associated with disease progression. Disseminated Intravascular Coagulation (DIC), an acquired and potentially fatal coagulation disorder, can arise with metastatic prostate cancer.
An 89-years-old male with metastatic adenocarcinoma of the prostate presented to the emergency department (ED) due to intermittent spontaneous bleeding from the right anterior lower extremity (RLE) and right posterior forearm (RUE) that started as a contusion 1 week prior. Physical exam revealed multiple ecchymoses on bilateral upper extremities, and upper quadrant regions secondary to a fall, and a bleeding wound on the RLE. The patient denied any epistaxis, hematuria, hematochezia, chest pain, shortness of breath, rash, or petechiae. Labs revealed WBC 7.6, hemoglobin 11.0, hematocrit 32.8, platelet 156, aPTT 38.5, PT 16.7, INR 1.45, D-Dimer 47.07, and fibrinogen 86. He was started on 2 units of cryoprecipitate and a q8h DIC panel.
During the hospital stay, multiple bleeding events from RLE and epistaxis were noted, and labs revealed worsening DIC panel. His PSA increased from 25.0 to 47.6 ng/mL in 2 weeks. Subsequently, he received 1 dose of docetaxel 100 mg. Throughout his stay of 8 days, he received a total of 14 units of cryoprecipitate and 3 units of fresh frozen plasma (FFP). Day 4 post-discharge, labs revealed aPTT 26.9, PT 13.3, INR 1.15, D-Dimer 11.28, and fibrinogen 220.
This case illustrates treating the causative factor of DIC is the best treatment. Early recognition and treatment are crucial and can be lifesaving for acute severe bleeding secondary to cancer. Supportive treatment should be promptly started and can be given to manage coagulopathy. However, it should not be used as the primary mean of treatment. The promising outcome of this treatment highlight the importance of chemotherapy to improve survival.
9:00 am Poster #5 – Case
CASE REPORT: To Bleed or Not to Bleed, That is DIC; A Closer Look at DIC in Metastatic
Prostate Cancer Treated with Docetaxel
Shabrina Jarrell – Medical School - WVU
Preceptor: Molly John, MD
9:00 am Poster E – Original
ORIGINAL: Azithromycin 5-day Versus 3-Day Course for Community Acquired Pneumonia:
A Non-Inferiority Trial
Austin Willett, PharmD - Pharmacy
Preceptor: Michael Czupryn, PharmD
Title:Azithromycin 5-day versus 3-day course for community-acquired pneumonia: A non-inferiority trial
Authors: Austin Willett, PharmD; Anthony Carfagna, PharmD Candidate 2023; Stacie Deslich, MA, MSHCA; Michael Czupryn, PharmD, BCPS
Purpose: Azithromycin is one portion of the standard empiric therapy for bacterial community-acquired pneumonia (CAP). Current guidelines make no formal recommendation on treatment duration in CAP. This study aimed to determine if a three-day course of azithromycin is non-inferior to a five-day course for CAP treatment.
Methods: Patients admitted to Charleston Area Medical Center between March 31, 2021 to March 31, 2022 diagnosed with CAP were identified via ICD-10 codes. Patients ≥18 years of age were analyzed for treatment with azithromycin 500 milligrams for five days or more versus three days. The primary composite outcome included the following: number of patients febrile after last day of treatment with azithromycin, number of patients requiring escalation of care to an intensive care unit after last day of treatment with azithromycin, and number of patients re-admitted within 30 days with CAP as the primary diagnosis. The non-inferiority margin was set at a 12.5% difference as described in the FDA’s guidance – Community-Acquired Bacterial Pneumonia: Developing Drugs for Treatment.
Results: Medical records of 174 patients were analyzed. Baseline demographics were similar between groups. Azithromycin 500 milligrams was received for five days or more in 97 patients and three days in 77 patients. The primary composite outcome demonstrated no statistical difference between groups (12/97 vs 12/77, p=0.3727). A statistical difference was observed between groups in hospital length of stay (8.7 vs 7.3 days, p=0.0339).
Conclusion: Our study demonstrated no statistical difference between five or more days versus three days of azithromycin 500 milligrams for the treatment of CAP; however, patients receiving five days of azithromycin were observed to have a longer hospital length of stay. Current guidelines make no formal recommendation on treatment duration with azithromycin in CAP. Our study suggests larger randomized controlled trials be conducted to confirm or refute our findings.
9:00 am Poster E – Original
ORIGINAL: Azithromycin 5-day Versus 3-Day Course for Community Acquired Pneumonia:
A Non-Inferiority Trial
Austin Willett, PharmD - Pharmacy
Preceptor: Michael Czupryn, PharmD
9:10 am Poster #6 – Case
CASE REPORT: Vulvar Hematoma Presenting as Bartholin's Cyst
Landon Foulger, DO – Obstetrics and Gynecology
Preceptor: Karinna Andrews, DO
Synovial sarcomas are relatively rare malignancies derived from pluripotent stem cells, and account for only 5-10% of all soft tissue sarcomas. The average age of onset is 39 years and affects both sexes equally. The majority of synovial sarcomas arise in the extremities, but can occur anywhere in the body. Vulvar location of these sarcomas are exceedingly rare, and only a handful of case reports have been described in the literature. We report a case of Synovial Sarcoma of the Vulva presenting as a painful vulvar lesion. The patient initially presented with a a vulvar cyst and dyspareunia. She underwent resection of the mass at an outlying facility in 2020 showing benign fibroadipose tissue. Two years later patient developed a recurring cyst in the area of prior resection and was referred to our facility for removal. She underwent an excision of a mons cyst, and pathology returned as a synovial sarcoma involving fibroconnective tissue extending to margins. The patient’s case was discussed at tumor board with consensus being to re-excise the lesion for negative margins. Patient subsequently underwent a partial radical vulvectomy with benign pathology. Patient is currently being managed expectantly for recurrence. This case and associated literature review is presented to add to the body of knowledge regarding synovial sarcomas of the female reproductive tract.
9:10 am Poster #6 – Case
CASE REPORT: Vulvar Hematoma Presenting as Bartholin's Cyst
Landon Foulger, DO – Obstetrics and Gynecology
Preceptor: Karinna Andrews, DO
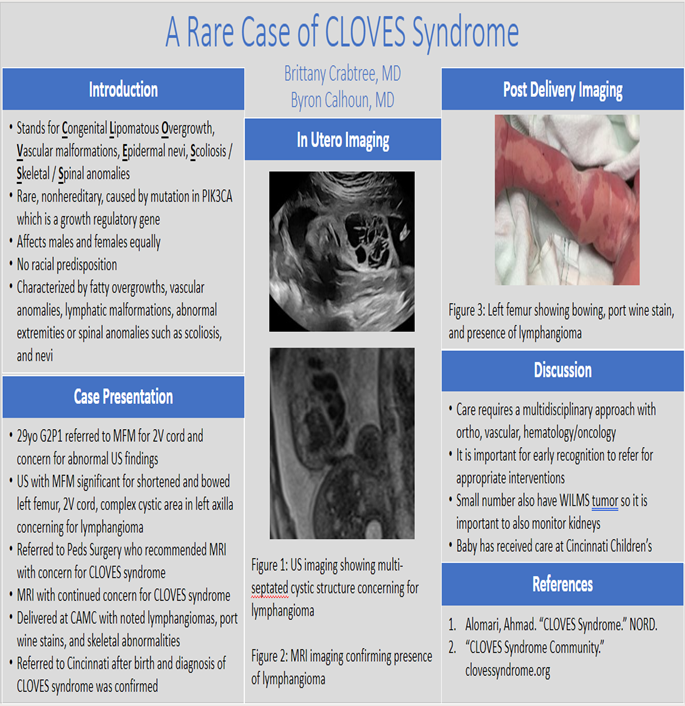
9:20 am Poster #7 – Case
CASE REPORT: CLOVES Syndrome
Brittany Crabtree, MD – Obstetrics and Gynecology
Preceptor: Byron Calhoun, MD
Introduction:
CLOVES syndrome is a rare disorder characterized by tissue overgrowth and vascular malformations. It is a nonhereditary disorder caused by mutation in a gene known as PIK3CA, a growth regulatory gene. CLOVES stands for congenital lipomatous overgrowth, vascular malformations, epidermal nevi and scoliosis/skeletal/spinal anomalies. It affects males and females equally with no racial predisposition. It is diagnosed at birth based on examination, with testing for the gene mutation.
The soft fatty masses of variable size located in the back, flanks, axilla, abdomen and buttocks. These masses may affect one or both sides of the body. The skin over the mass is typically covered with a red-pinkish birthmark. The vascular anomalies are associated with dilated veins in the chest, upper and lower extremities may cause clot formation and occasionally serious pulmonary embolism. Lymphatic malformations are abnormal, large spaces filled with lymph. These malformations are frequently noted within the fatty masses or in the abdomen, chest and extremities. A small subgroup of patients may suffer from the more aggressive arteriovenous malformation around the area of the spinal cord. Abnormal extremities (arms and legs) are common. Large wide hands or feet, large fingers or toes, wide space between digits (sandal gap toe) and uneven size of extremities are common.Spinal anomalies include scoliosis (curving of the spine), fatty masses and vessels pushing on the spinal cord and tethered cord (spinal cord fixed by abnormal band). Skin birthmarks include port-wine stains, prominent veins, lymphatic vesicles, moles and epidermal nevus (slightly raised areas of skin with light brownish color). Lastly, kidney anomalies can include size of the kidneys could be asymmetric (one is larger) and may show some abnormal features on imaging studies. Wilms tumor has been noted in a small number of young patients with CLOVES syndrome. This requires screening with serial ultrasound examinations during childhood. Additional findings can occur in CLOVES syndrome including bleeding from the intestine, urinary bladder and asymmetric face and head.
Case:
Our patient was a 29yo female G2P1001 who was referred to the MFM for 2 vessel cord and some possible abnormalities seen on US. She presented for a genetic US. It was significant for a shortened and bowed left femur, 2V cord, and a complex cystic area in the left axilla extending to the superior portion of the abdomen measuring 5.8 x 2.4 x 2.7cm. This area was concerning for a lymphangioma. The patient was referred to pediatric surgery who recommended an MRI with concern for CLOVES syndrome. MRI returned with continued concern for CLOVES Syndrome. Baby was delivered at CAMC and noted to have lymphangiomas and port wine stains over much of her body. After birth, baby was referred to Cincinnati Children’s Hospital where the diagnosis of CLOVES was confirmed.
Management is multidisciplinary and often requires surgical teams specialized in orthopedics for limb anomalies, debulking for tissue anomalies, vascular surgery for malformations, as well as some medical management with antineoplastic agents such as sirolimus managed by heme-onc. It is important for early recognition and consult with centers specializing in care for this complicated syndrome.
9:20 am Poster #7 – Case
CASE REPORT: CLOVES Syndrome
Brittany Crabtree, MD – Obstetrics and Gynecology
Preceptor: Byron Calhoun, MD
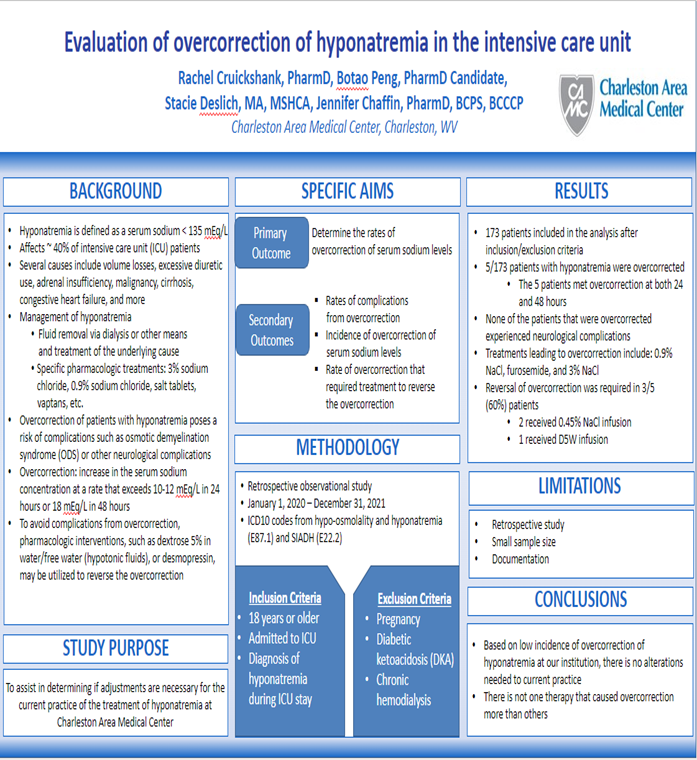
9:20 am Poster G – Original
ORIGINAL: Evaluation of Overcorrection of Hyponatremia in the Intensive Care Unit
Rachel Cruickshank, PharmD - Pharmacy
Preceptor: Jennifer Chaffin, PharmD
OBJECTIVE
Empiric observation of patients treated with a standardized fluid and electrolyte replacement protocol shows frequent need to alter composition of IV fluids to correct hypokalemia, hypophosphatemia and hyperchloremia. We hypothesize that quantitively describing the frequency and nature of IV fluid changes and electrolyte abnormalities that prompt those changes may inform the design of empiric fluids. This could minimize the frequency of electrolyte abnormalities and fluid changes during DKA therapy.
METHODS
This was a retrospective descriptive study of patients admitted to the pediatric ICU with a diagnosis of DKA between September 2016 and December 2021 who were treated with current institutional protocol fluids. If a patient was started on the institutional fluid protocol, their initial, lowest, and highest serum values for sodium, potassium, chloride, magnesium, and phosphate were recorded. These patients were then examined to see whether these fluctuations resulted in IV fluid alterations or electrolyte supplementation.
RESULTS
There were 308 children included in the analysis. Of the patients that received the protocol fluids initially, 40% had changes made to their IV fluids. In patients included in the analysis, 40% developed hyperchloremic metabolic acidosis. The most common changes in fluids were a decrease in chloride (31%) and an increase in phosphate (28%).
CONCLUSIONS
Based on the results of this study, a significant number of patients in DKA treated with the protocol fluids required fluid changes during therapy. These data suggest that DKA resuscitation fluids should contain less than 97 mEq/L chloride and more than 14 mmol/L phosphate.
9:20 am Poster G – Original
ORIGINAL: Evaluation of Overcorrection of Hyponatremia in the Intensive Care Unit
Rachel Cruickshank, PharmD - Pharmacy
Preceptor: Jennifer Chaffin, PharmD
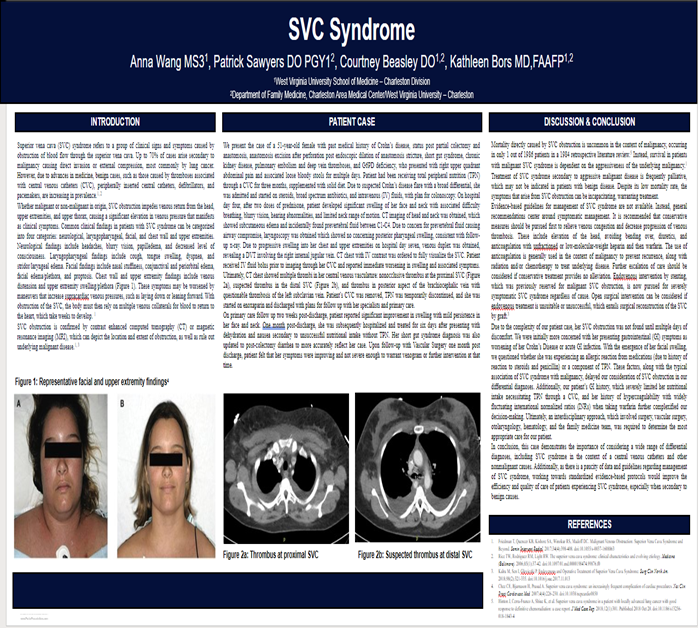
9:50 am Poster #8– Case
CASE REPORT: SVC Syndrome
Anna Wang – Medical Student – WVU
Preceptor: Courtney Beasley, DO
Superior vena cava (SVC) syndrome refers to a group of clinical signs and symptoms caused by obstruction of blood flow through the SVC. Most cases arise secondary to malignancy but can also be central venous device-related.
A 51-year-old female presented with abdominal pain and loose stools for multiple days. She has a history of Crohn’s disease with multiple abdominal surgical procedures, short gut syndrome, pulmonary embolism, and deep vein thrombosis (DVT). Patient had been receiving total parenteral nutrition (TPN) through a central venous catheter (CVC) for three months. Due to suspected Crohn’s disease flare with a broad differential, she was admitted and started on steroids, broad spectrum antibiotics, and intravenous (IV) fluids, with plan for colonoscopy. After two doses of prednisone, patient developed significant swelling in her face and neck with associated difficulty breathing, blurry vision, hearing abnormalities, and limited neck range of motion. Due to progressive swelling into her chest and upper extremities, venous duplex was obtained, revealing a DVT involving the right internal jugular vein. Computed tomography (CT) chest with IV contrast was ordered to fully visualize the SVC. Patient received IV fluid bolus prior through her CVC and reported immediate worsening in swelling and associated symptoms. CT chest showed multiple thrombi in central venous vasculature. CVC was removed, TPN was temporarily discontinued, and patient was started on enoxaparin and discharged with plans for follow-up.
This case demonstrates the importance of considering a wide range of differential diagnoses. Due to a history of swelling after steroid use, multiple drug allergies, and medical complexity, her SVC syndrome diagnosis was delayed in favor of more overt explanations. Additionally, as there is a paucity of data and guidelines regarding management of SVC syndrome, working towards standardized diagnostic and treatment protocols would improve the efficiency and quality of care of patients experiencing SVC syndrome.
9:50 am Poster #8– Case
CASE REPORT: SVC Syndrome
Anna Wang – Medical Student – WVU
Preceptor: Courtney Beasley, DO
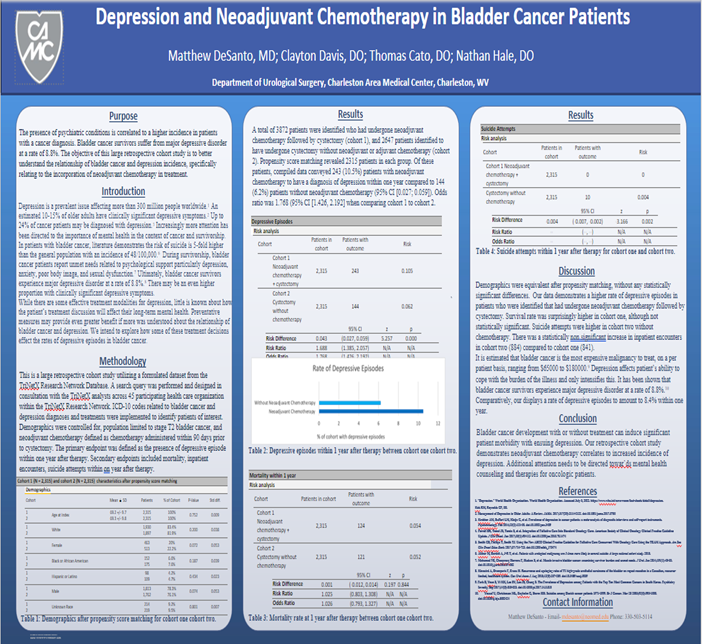
9:50 am Poster H – Original
ORIGINAL: Depression and Perioperative Chemotherapy in Bladder Cancer Patients
Matthew DeSanto, MD – Urological Surgery
Preceptor: Nathan Hale, DO
Introduction: The objective of this large retrospective cohort study is to better understand the relationship of bladder cancer and depression incidence, specifically relating to the incorporation of perioperative chemotherapy in treatment.
Methods: This is a large retrospective cohort study utilizing a formulated dataset from the TriNetX Research Network Database. A search query was performed and designed in consultation with the TriNetX analysts across 45 participating health care organization within the TriNetX Research Network. ICD-10 codes related to bladder cancer and depression diagnoses and treatments were implemented to identify patients of interest. Demographics were controlled for, population limited to stage T2 bladder cancer, and perioperative chemotherapy defined as within 90 days prior to cystectomy.
Results: A total of 3872 patients were identified with perioperative chemotherapy followed by cystectomy (cohort 1), and 2647 patients identified to have undergone cystectomy without neoadjuvant or adjuvant chemotherapy (cohort 2). Propensity score matching revealed 2315 patients in each group. Of these patients, preliminary data conveyed 243 (10.5%) patients with perioperative chemotherapy to have a diagnosis of depression within one year compared to 144 (6.2%) patients without perioperative chemotherapy (95% CI [0.027; 0.059]). Odds ratio was 1.768 (95% CI [1.426, 2.192] when comparing cohorts 1 to cohort 2.
Conclusion: Bladder cancer development with or without treatment can induce significant patient morbidity with ensuing depression. Our retrospective cohort study demonstrates perioperative chemotherapy correlates to increased incidence of depression. Additional attention needs to be directed towards mental health counseling and treatment for oncologic patients.
9:50 am Poster H – Original
ORIGINAL: Depression and Perioperative Chemotherapy in Bladder Cancer Patients
Matthew DeSanto, MD – Urological Surgery
Preceptor: Nathan Hale, DO
10:00 am Poster #9- Case
CASE REPORT: Acute Onset Hyperbilirubinemia in a Patient Taking Aranesp
for Myelodysplastic Syndrome
Rachel Martin, MD – Emergency Medicine
Preceptor: Andrew Morgan, DO
A 71-year-old Caucasian female presents to the emergency department with sudden-onset jaundice. Patient has a history of myelodysplastic syndrome and recently started Aranesp (darbopoetin alfa), an erythropoesis stimulating agent, approximately one week prior to presentation. On exam, patient had severe jaundice and normal mentation. Labs showed normocytic anemia, indirect hyperbilirubinemia, and normal liver enzyme levels. Additional labs including lactate dehydrogenase, serum haptoglobin, iron panel, transferrin, Coombs test, and peripheral blood smear were pending at time of disposition to inpatient admission. Patient was provided blood product in the emergency department. Differential diagnosis at that time included symptomatic anemia vs. hemolytic anemia vs. paroxysmal nocturnal hemoglobinuria vs indirect hyperbilirubinemia of uncertain etiology. Throughout admission, the patient was believed to have indirect hyperbilirubinemia of uncertain etiology due to non-elevated serum haptoglobin and lactate dehydrogenase. Aranesp belongs to the pharmacologic class of colony stimulating factors and is an erythropoiesisstimulating agent. Because of its mechanism of action, it is useful in cases of anemia, commonly associated with chemotherapeutic effects or chronic renal disease. Studies have also shown that it is beneficial in lower risk myelodysplastic syndromes for management of symptomatic anemia. Due to the increase in blood cells that Aranesp causes, the majorly reported adverse effects are hypertension and thrombotic events. Although other side effects have been recorded, there are currently no documented cases of jaundice, hepatotoxicity, hemolysis, or hyperbilirubinemia that would explain the patient's presentation. While Aranesp may not be the cause of the patient's symptoms and the association may be coincidental, there is the possibility that this could be the first case of jaundice due to hyperbilirubemia associated with Aranesp use was reported.
10:00 am Poster #9- Case
CASE REPORT: Acute Onset Hyperbilirubinemia in a Patient Taking Aranesp
for Myelodysplastic Syndrome
Rachel Martin, MD – Emergency Medicine
Preceptor: Andrew Morgan, DO
10:00 am Poster I – Original
ORIGINAL: Contemporary Surgical Management of Advanced Renal Cell Carcinoma with
Venous Extension: Does Timing of Pre-operative Imaging Make a Difference?
Jordon Burns, DO – Urological Surgery
Preceptor: Nathan Hale, DO
Authors: Jordan Burns, D.O., Stacie Deslich, M.A., M.S., Nathan Hale, D.O., Samuel Deem, D.O.; Charleston Area Medical Center Department of Urology, Charleston, WV; Charleston Area Medical Center Institute for Academic Medicine, Charleston, WV.
Purpose: Advanced renal cell carcinoma (RCC) can be associated with tumor thrombus formation within the renal vein, vena cava, and right atrium. Accurate preoperative assessment of the level tumor thrombus extension is important for surgical planning. The time between initial diagnosis and tumor thrombus progression is unclear. The objective of this study was to determine if there is an optimal window to obtain cross-sectional imaging prior to surgery to best characterize the level of thrombus extension with the goal of minimizing unplanned intraoperative events and improving patient outcomes.
Methods: This study was a retrospective analysis of patients with stage pT3 kidney cancer treated with radical nephrectomy at two institutions from March 1, 2010, to February 28, 2019. Patient charts were reviewed, and data gathered included demographic information and medical, surgical and treatment information for patients meeting inclusion criteria. Statistical analysis was then performed to determine if there was an optimal window prior to surgery to characterize the level of thrombus extension.
Results: Preliminary results indicate that imaging greater than 19 days prior to surgery led to increased consultations and complications (p-value 0.004 and p-value 0.01 respectively). No significant differences were noted for operative time, blood loss, transfusion, Clavien III-IV complications or length of stay.
Conclusions: Preoperative imaging of the level of tumor thrombus extension is most effective when it is performed within 19 days prior to surgery. Longer time windows between imaging and the operation led to less desirable outcomes.
10:00 am Poster I – Original
ORIGINAL: Contemporary Surgical Management of Advanced Renal Cell Carcinoma with
Venous Extension: Does Timing of Pre-operative Imaging Make a Difference?
Jordon Burns, DO – Urological Surgery
Preceptor: Nathan Hale, DO
10:10 am Poster J - Original
ORGINAL: Fixed Dose 4-Factor Prothrombin Complex Concentrate for the Reversal of
Factor Xa Inhibitors
Matthew Richardson, PharmD - Pharmacy
Preceptor: Mathew Johnson, PharmD
Purpose: Oral factor Xa inhibitors have become increasingly popular. One agent that is utilized for the reversal of factor Xa inhibitors is 4-factor prothrombin complex concentrate (4F-PCC). Studies have examined weight-based and fixed dose strategies for 4F-PCC. Charleston Area Medical Center transitioned to fixed dose 4F-PCC on December 21, 2021.
Methods: This was a retrospective cohort study that assessed the efficacy of fixed dose 4F-PCC versus weight-based dosing for the reversal of factor Xa inhibitors due to a bleeding event between June 1, 2020 and August 31, 2022. The weight-based arm utilized a dose of 25 to 50 units/kg. For the fixed dose arm, patients less than 100 kg received 2000 units, while those greater than or equal to 100 kg received 2,500 units. Patients could receive a supplemental dose of 500 units if deemed necessary by the provider. Patients were excluded if they were less than 18 years old, pregnant, not taking an oral factor Xa inhibitor, received another reversal agent, or did not experience a bleeding event.
Results: The fixed dose group (n = 57) had a hemostasis rate of 53% compared to 44% for the weight-based group (n =70) (p=0.35). In-hospital mortality was higher in the weight-based group (29% vs 11%, p=0.01). Hospital length of stay and incidence of VTE were similar between groups. In a subgroup analysis, patients that received a weight-based dose less than 35 mg/kg had higher mortality than those in other groups (p=0.03). Outcomes were not significant when patients were stratified by bleeding location. Utilizing fixed dose 4F-PCC reduced cost by an estimated $39,418 per year.
Conclusions: This study found no difference in hemostasis between weight-based and fixed dose 4F-PCC. Although mortality was lower in the fixed dose group, this was likely due to chance or confounding factors. This study supports the decision to switch from weight-based dosing to fixed dosing of 4F-PCC.
10:10 am Poster J - Original
ORGINAL: Fixed Dose 4-Factor Prothrombin Complex Concentrate for the Reversal of
Factor Xa Inhibitors
Matthew Richardson, PharmD - Pharmacy
Preceptor: Mathew Johnson, PharmD
10:20 am Poster K – Original
ORIGINAL: Patient and Provider Experience with Telehealth Visits in a Family Medicine Center
Lucas Goodwin, DO – Family Medicine
Preceptor: Andy Tanner, DO
Authors: Jeffrey Ashley MD, Andy Tanner DO, Lucas Goodwin DO, Emily Rider DO, Lisa Calderwood MPH
Purpose: COVID-19 created many challenges for healthcare providers including the use of telemedicine. Telehealth allowed safe care through social distancing but created questions regarding overall quality of care patients received.
Methods: This study looks at different variable from both patient and provider perspectives, creating feedback to identify both strengths and weaknesses of telemedicine. 55 patients, 18 years or older, and 16 providers that participated in telemedicine at the CAMC Family Medicine Center (FMC) from January 1, 2020 through December 1, 2020, completed surveys. Patients were provided a paper survey, to be completed and returned at their discretion. Providers were emailed the link to a survey in REDCap. Both surveys focused on identifying satisfaction, sufficiency, and if they had ever used Telemedicine prior to the pandemic.
Results: There was no statistical difference in patients’ perception of communication with their provider based
on the use of video with their call (p=0.30). A Fisher’s exact test of independence showed that there was no significant association in patient preference for in person vs telemedicine and the acute need for their visit (p=0.83). There was no difference in reported patient perception of communication with provider based on insurance type (p=0.56). There was no association between patient’s gender and communication with provider (p=1.00). There was no association between visit satisfaction and telemedicine training received (p=1.00). There was no association between visit satisfaction and level of employment: faculty physician vs resident physician (p=0.06).
Conclusion: Telemedicine continues to transform the ability we have to practice medicine and provide safe and quality care to our patients. The data findings were not significant; however, with increased sample size significance would likely be observed. Without significantly negative findings, this could suggest that telehealth is perceived as useful as traditional office visits.
10:20 am Poster K – Original
ORIGINAL: Patient and Provider Experience with Telehealth Visits in a Family Medicine Center
Lucas Goodwin, DO – Family Medicine
Preceptor: Andy Tanner, DO
10:30 am Poster L – Original
ORIGINAL: Outcomes Following Same Day Discharge Post-RALP in the Post-COVID19 Era
Mary Novak, DO – Urological Surgery
Preceptor: Samuel Deem, DO
Purpose: Robotic assisted laparoscopic radical prostatectomy (RALP) is a commonly performed
procedure for the treatment of prostate cancer, and is currently being performed by two urologic oncologists in our institution almost daily. Traditionally patients have been admitted to the hospital for overnight observation following their prostatectomy, however more recent trends have encouraged offering same day discharge following this robotic procedure. Same day discharge was offered by our institution prior to the COVID19 pandemic, however during the pandemic it became more readily accepted by patients due to hospital restrictions and to avoid delays in cancer treatment. Our study aims to evaluate CAMC’s experience with same day discharge following RALP by evaluating incidence of readmission and complications following same day discharge vs. overnight hospital stay. It also seeks to identify risk factors related to failure of same day discharge.
Methods: Data collection was performed for patients undergoing robotic assisted prostatectomy from March 2020 – June 2022. Patient demographics and other variables including operative time, BMI, ASA Score, etc. were evaluated. The rate of complications and readmission within 30 and 90 days were compared between patients electing day discharge and those electing overnight hospital stay.
Results: We identified 205 patients undergoing RALP in the post-COVID19 pandemic era. Our preliminary data reveal that there is no difference in complication and readmission rates between same day discharge and overnight observation cohorts, with readmission rate of approximately 14% in each cohort. BMI is the only variable found to correlate to increased risk of complications and readmissions. Average BMI in the patients was found to be approximately 30, while the average BMI in the same day discharge cohort was 28. Most parameters we investigated were approximately the same in the cohorts, however same day discharge cohort did report less blood loss compared to the overnight stay cohort.
Conclusions: Overall, same day discharge following robotic prostatectomy does not increase complications or readmission rates compared to overnight observation. However, increased BMI is correlated to increased complication and readmission rate. Further analysis of same day discharge data can help surgeons identify the ideal candidates for same day discharge following robotic surgeries.
10:30 am Poster L – Original
ORIGINAL: Outcomes Following Same Day Discharge Post-RALP in the Post-COVID19 Era
Mary Novak, DO – Urological Surgery
Preceptor: Samuel Deem, DO
10:40 am Poster #13 – Case
CASE REPORT: A Case of Synovial Sarcoma of the Vulva
Jessica Allen, MD – Obstetrics and Gynecology
Preceptor: Stephen Bush, II, MD
A Case of Synovial Sarcoma of the Vulva Synovial sarcomas are relatively rare malignancies derived from pluripotent stem cells, and account for only 5-10% of all soft tissue sarcomas. The average age of onset is 39 years and affects both sexes equally. The majority of synovial sarcomas arise in the extremities, but can occur anywhere in the body. Vulvar location of these sarcomas are exceedingly rare, and only a handful of case reports have been described in the literature. We report a case of Synovial Sarcoma of the Vulva presenting as a painful vulvar lesion. The patient initially presented with a a vulvar cyst and dyspareunia. She underwent resection of the mass at an outlying facility in 2020 showing benign fibroadipose tissue. Two years later patient developed a recurring cyst in the area of prior resection and was referred to our facility for removal. She underwent an excision of a mons cyst, and pathology returned as a synovial sarcoma involving fibroconnective tissue extending to margins. The patient’s case was discussed at tumor board with consensus being to re-excise the lesion for negative margins. Patient subsequently underwent a partial radical vulvectomy with benign pathology. Patient is currently being managed expectantly for recurrence. This case and associated literature review is presented to add to the body of knowledge regarding synovial sarcomas of the female reproductive tract.
10:40 am Poster #13 – Case
CASE REPORT: A Case of Synovial Sarcoma of the Vulva
Jessica Allen, MD – Obstetrics and Gynecology
Preceptor: Stephen Bush, II, MD
10:50 am Poster N – Original
Implementation and Outcomes of a Single-Site CAUTI SUR Management Protocol
Carly Ulrich, DO
Preceptor: Ryan Fitzwater, DO
Purpose: Catheter associated urinary tract infections (CAUTI) have long been a source of hospital acquired infections that can be controlled and decreased through the implementation of management protocols and processes. Current literature suggests that programs based on the Plan Do Study Act cycle, focused multidisciplinary rounding, Kamishibai cards and daily tracking of catheter insertion, use and removal have been effective in decreasing both the Standardized Utilization Rate (SUR) and the Standardized Infection Rate (SIR). This research attempted to identify best practices for CAUTI prevention via the use of multidisciplinary rounding and Kamishibai card use in a single site institution. Findings will be useful in continuing to determine and implement appropriate and effective catheter utilization.
Methods: Medical records of 300 patients admitted to the trauma and neurological care floor of a single institution between January 1, 2019, and December 31, 2021 who also received an indwelling catheter were reviewed. Data collected from medical, surgical, and operative records included demographic information as well as procedure, length of stay and infection rates and treatment.
Results: Preliminary results indicated that of the 300 patient records reviewed, 98 were part of the Kamishibai card tracking. Those patients in the treatment group had 22.5% fewer CAUTI infections than those in the control group (p<0.001).
Conclusions: CAUTI continues to be a source of hospital acquired infections, and this study indicated that the implementation of Kamishibai cards in patient care and catheter tracking has a positive effect on patient health by significantly reducing CAUTI rates. Kamishibai can be included in best practices for CAUTI prevention and treatment for patients with indwelling catheters.
10:50 am Poster N – Original
Implementation and Outcomes of a Single-Site CAUTI SUR Management Protocol
Carly Ulrich, DO
Preceptor: Ryan Fitzwater, DO
11:00 am Poster #15 - Case
CASE REPORT: Acquired Bronchoesophageal Fistula
Caitlin Mulvihill, MD – Emergency Medicine
Preceptor: Amy Hunt, DO
A 36-year-old male, with a recent diagnosis of metastatic esophageal cancer status post esophageal stent placement 2.5 weeks ago, presented to the emergency department complaining of hematemesis beginning this morning. The patient had presented a week prior complaining of a persistent cough and shortness of breath and was subsequently diagnosed with pneumonia and started on an antibiotic. This visit, the patient was hypoxic on arrival to the ED and started on supplemental oxygen via nasal cannula. Patient met sepsis criteria and sepsis protocol was initiated. CTA of the chest was performed and was concerning for an esophageal rupture. The case was discussed with cardiothoracic surgery who performed further imaging that showed no extravasation of contrast and no rupture. While in the ED, the patient decompensated and was intubated for airway protection. Patient was admitted to the ICU where a bronchoscopy was performed which showed a broncho-esophageal fistula in the left main stem. Pulmonology placed an endobronchial stent during repeat bronchoscopy. Patient has poor prognosis and was discharged with Hospice. A broncho-esophageal fistula is an anomalous communication between the bronchi and esophagus. They can be either congenital or acquired (greater than 50% of cases). Most acquired cases, such as this one, are caused by malignant tumor invasion. They are also commonly caused by endoscopic intervention, post-intubation trauma, chronic infection such as tuberculosis, or foreign bodies. 5-15% of patients with esophageal cancer develop a bronchi-esophageal fistula. Patients typically present with frequent coughing, fever, recurrent pneumonia and aspiration, and unexplained malnutrition. Diagnostic evaluation is similar to previously discussed with CTA, esophagram, and bronchoscopy.
Due to the diverse range of causes, physicians must have a high index of suspicion in patients with symptoms concerning for fistula as, when left untreated, outcomes are generally poor. Initial management includes treatment of aspiration pneumonia, stopping oral intake, elevating the head of the bed, supplemental oxygen and starting anti-reflux therapy. Benign, symptomatic fistulas are typically treated with surgery. Malignant broncho-esophageal fistulas are generally treated with palliative endo/bronchoscopy treatments such as stenting if the deformity is large enough.
11:00 am Poster #15 - Case
CASE REPORT: Acquired Bronchoesophageal Fistula
Caitlin Mulvihill, MD – Emergency Medicine
Preceptor: Amy Hunt, DO
11:20 am Poster #17 – Case
CASE REPORT: MAC Attack - The Curious Case of Hypercalcemia in a Patient With AIDS,
Disseminated MAC Infection, and DRESS Syndrome
Tajana Juranovic, MD – Internal Medicine
Preceptor: A. Durden Witt, DO
Introduction: In most patients, hypercalcemia is due to either primary hyperparathyroidism or malignancy. The degree of hypercalcemia helps to differentiate these two mechanisms, levels above 11.5 mg/dL are most associated with malignancy. However, severe hypercalcemia has other causes that must be considered, as our case demonstrates.
Case presentation: We present a case of a 30-year-old male with AIDS and MAC infection who presented with nausea, vomiting, and morbilliform rash. He was found to have hypercalcemia of 14.2 mg/dL, acute kidney injury, low PTH, normal vitamin D, elevated ferritin at 4023 ng/ml, and elevated 1,25-vitamin D of 114 pg/L. His CD4 count was 32, and his HIV viral load was undetectable. Abdominal CT scan showed hepatosplenomegaly and retroperitoneal lymphadenopathy. Lymph node and bone marrow biopsy did not show the presence of lymphoma or other malignancy but showed the presence of histiocytes with intracellular clusters of acid-fast bacilli. The bone scan was without osteolytic lesions. He was treated aggressively with fluids and corticosteroids after discovering that his rash developed 6 weeks after ethambutol initiation and was consistent with DRESS syndrome.
Discussion: This case presented a significant diagnostic challenge given the patient’s medical complexity with AIDS, MAC infection, DRESS Syndrome, lymphadenopathy, splenomegaly, and weight loss. Differential diagnoses for hypercalcemia include granulomatous infection, secondary malignancy, primary hyperparathyroidism, drugs, and immune reconstitution syndrome in patients with AIDS. Ultimately this patient was diagnosed with severe hypercalcemia secondary over production of 1,25 dihydroxy vitamin D due to disseminated MAC infection confirmed by tissue biopsy. Determining how to treat the hypercalcemia was a difficult decision as well due to the different treatment strategies for hypercalcemia of malignancy versus granulomatous disease. Treatment for hypercalcemia due to granulomatous diseases often incorporates glucocorticoids. Our patient was initially treated with prednisone for his rash which serendipitously treated his hypercalcemia as well.
11:20 am Poster #17 – Case
CASE REPORT: MAC Attack - The Curious Case of Hypercalcemia in a Patient With AIDS, Disseminated MAC Infection, and DRESS Syndrome
Tajana Juranovic, MD – Internal Medicine
Preceptor: A. Durden Witt, DO
11:30 am Poster #18 – Case
CASE REPORT: A Strong COPD Exacerbation
Brandon Howe, MD – Internal Medicine
Preceptor: Emily Fridenmaker, MD
Introduction: Strongyloides stercoralis is a parasitic round worm that is known to cause human infection in endemic areas, particularly in the immunocompromised. Infection has been known to occur years following exposure and can be lifelong if left untreated. Endemic areas in the United States include areas with sub-tropical weather and areas with poor sanitation.
Case presentation: A 70-year-old man with a history of advanced COPD, asbestosis, and chronic hypoxic respiratory failure presented with worsening cough, increased sputum purulence, and dyspnea for four days. He was recently discharged for a COPD exacerbation, treated with prednisone and azithromycin. He had a 41-pack year smoking history and was a military veteran who served in the Vietnam war but had lived in West Virginia for most of his life. On exam, end expiratory wheezes were present bilaterally and he was using his baseline oxygen requirement of 4 liters per minute. Laboratory was significant for leukocytosis of 12.7 x 109/L, with an absolute eosinophil count of 760/mL. Chest CT revealed Bilateral ground glass opacities with subpleural sparing with signs of prior asbestos exposure and prior granulomatous disease. Sputum culture was positive for strongyloides stercorali.
Discussion: It is suspected that this patient had a prior exposure to strongyloides, with hyperinfection resulting from multiple subsequent courses of steroids. It is possible that his initial exposure occurred in Vietnam, but strongyloides is also endemic to West Virginia. It is also feasible that his recurrent admissions for dyspnea were driven by untreated pulmonary strongyloidiasis, rather than recurrent COPD exacerbations. This patient did not receive preventative screening or treatment for strongyloides prior to receiving steroids. Data suggest that if individuals live in an endemic area and there is need for immunosuppressive therapy, serologic testing for strongyloides should be performed prior to initiation. If immunosuppressive therapy must be initiated urgently, it is recommended to treat empirically with ivermectin.
Conclusion: This case demonstrates the importance of having a high index of suspicion for strongyloidiasis when practicing in endemic areas. Patients living in endemic areas should undergo serologic testing or empiric treatment for strongyloidiasis prior to being treated with prolonged steroids or other forms of immunosuppression.
11:30 am Poster #18 – Case
CASE REPORT: A Strong COPD Exacerbation
Brandon Howe, MD – Internal Medicine
Preceptor: Emily Fridenmaker, MD
11:40 am Poster #19 – Case
CASE REPORT: Artery of Percheron Occlusion; A Rare Cause of Stroke!
Rabia Anees, MD – Internal Medicine
Preceptor: Khawaja Owais Omar, MD
Introduction:
The artery of Percheron (AOP) is a rare anatomical artery variant of the paramedian branches of the posterior cerebral artery (PCA) supplying the thalamus and rostral midbrain. The AOP branch from the PCA is one of the few single-artery pathologies that affect bilateral structures in the brain and results in permanent deficits.
Case:
A 59-year-old male with PMH of hypertension, diabetes, and prior CVA with hemianopsia due to occipital lobe infarct, presented with unconsciousness. The morning of presentation he was in a normal state of health, but was found unresponsive by evening and the duration of symptoms was unknown. No TPA was given. He was intubated by EMS. Brain CT scan was unremarkable. Head CTA showed no significant stenosis in distal internal carotid or cervical arteries. Normal vascular flow was observed in the anterior and middle circulation with distal vertebral and basilar arteries showing no evidence of stenosis, occlusions, or aneurysms. Left PCA included multifocal to severe stenosis, in addition to severe stenosis of right PCA in proximal P1 segment.MRI showed infarction of bilateral Thalami without large vessel occlusion. Thrombectomy was not done. EEG was negative for seizures. TEE was negative for thrombus. He regained consciousness, but was unable to follow commands. Due to poor mental status he was not extubated. Tracheostomy and Peg tube were placed. Cognitive deficits, global weakness and receptive and expressive aphasia persisted. Patient was discharged to a stroke rehab center with a modified Rankin scale of 5.
Discussion:
This case is unique as it accounts for only 0.1-2% of all strokes. It's important to consider stroke due to AOP occlusion in patients presenting with a triad of reduced GCS, memory impairment and gaze palsy. Identification with MRI in therapeutic windows for thrombolysis can be lifesaving as there are few cases of successful thrombolysis.
11:40 am Poster #19 – Case
CASE REPORT: Artery of Percheron Occlusion; A Rare Cause of Stroke!
Rabia Anees, MD – Internal Medicine
Preceptor: Khawaja Owais Omar, MD
11:50 am Poster #20 – Case
CASE REPORT: Not Factoring into Account Intrinsic Losses- A Case of Factor VII Deficiency
Borna Amir-Kabirian, MD – Internal Medicine
Preceptor: Amir Kamran, MD
Introduction: The coagulation cascade is a series of three pathways that lead to hemostasis and stabilization of a platelet plug. The intrinsic and extrinsic components lead to the same goal of activating fibrinogen to fibrin through the common pathway. Factor VII is a key component for the extrinsic pathway. Ordinarily, factor VIIa, the activated version of factor VII circulates in the blood stream. Upon encountering damaged tissue, tissue factor located in the subendothelium binds with factor VIIa. This activates factor XI to X from the common pathway, subsequently resulting in stabilization of the fibrin clot. In very rare instances, individuals can have an inherited factor VII deficiency, disrupting this process. We present a case of factor VII deficiency.
Case: A 62-year-old male presented to the ER due to an elevated INR discovered during pre-operative testing. He denied history of excessive bruising or bleeding and had recent spinal surgery without complications. On arrival, he had an elevated prothrombin time of 30, INR of 2.55 and partial thromboplastic time of 34. He received vitamin K without improvement of his PT/INR. Hepatic function and vitamin K levels returned normal. Liver ultrasound showed fatty infiltration. Further workup revealed correction of the INR on the mixing study, and a low factor VII without an inhibitor. He was diagnosed with factor VII deficiency.
Discussion: Inherited factor VII deficiency is characterized by a spectrum. Low risk patients have greater than 20% factor VII factors and are often asymptomatic. However, this raises the question of management pre-operatively. Should they receive pre- or intra-operative prophylaxis? In the STER trial conducted by Mariani et al, minor procedures were treated with replacement therapy in patients who had < 20% levels of factor VII. Similarly, recombinant factor VII with tranexamic acid was successfully used in the vaginal delivery of a prim gravid female with a history of factor VII deficiency. This case represents an opportunity to discuss benefits and risks of prophylaxis in patients with factor VII deficiency.
11:50 am Poster #20 – Case
CASE REPORT: Not Factoring into Account Intrinsic Losses- A Case of Factor VII Deficiency
Borna Amir-Kabirian, MD – Internal Medicine
Preceptor: Amir Kamran, MD
1:00 pm Poster #21 – Case
CASE REPORT: A Grave Matter Post Covid Infection
Parisa Aijaz, MD – Internal Medicine
Preceptor: Amna Anees, MD
Introduction: Since the emergence of the COVID-19 pandemic, there has been a surge of reports linking the effects of the virus with the development of autoimmune disorders, including the thyroid. The effect on thyroid gland ranges from hypothyroidism, hyperthyroidism, to subclinical abnormalities. Patients with a history of thyroid disease, or a genetic disposition may experience a more potent effect. Grave’s Disease (GD) is a rare complication that can occur from COVID-19. There have been some reports linking COVID-19 infection to either new onset or reactivation of GD. Individuals with a history of GD commonly present within 2 months after covid infection with an exacerbation.
Case: We present a case of a 42-year-old female with a history of GD who presented to the Emergency Department for an acute exacerbation of her hyperthyroidism symptoms, 3-weeks after her SARS-CoV-2 infection. Her symptoms included daily headaches, increased bilateral eye pressure, fatigue, muscle weakness, episodes of confusion and agitation, and persistent heart palpitations. On examination, she had a goiter. She had an elevated fT4 of 5.57, fT3 of 15.68, total T3 of 4.43, and near-absent TSH. Her Burch-Wartoskfy scale was 40, which was concerning for an impending thyroid storm however at the time of admission, she was not in thyroid storm. She was treated with PTU, SSKI, and propranolol, with improvement in her symptoms. Due to her prior history of intolerance to antithyroid medications and her recent exacerbation of symptoms, she underwent thyroidectomy during admission once she was in euthyroid state.
Discussion: Our case demonstrates the importance of recognizing COVID-19 as an etiology or a trigger for new onset or reactivation of GD. Even though our patient presented with typical features of GD, this case highlights the importance of being vigilant to recognize this association between COVID-19 and thyroid abnormalities for early diagnosis and treatment.
1:00 pm Poster #21 – Case
CASE REPORT: A Grave Matter Post Covid Infection
Parisa Aijaz, MD – Internal Medicine
Preceptor: Amna Anees, MD
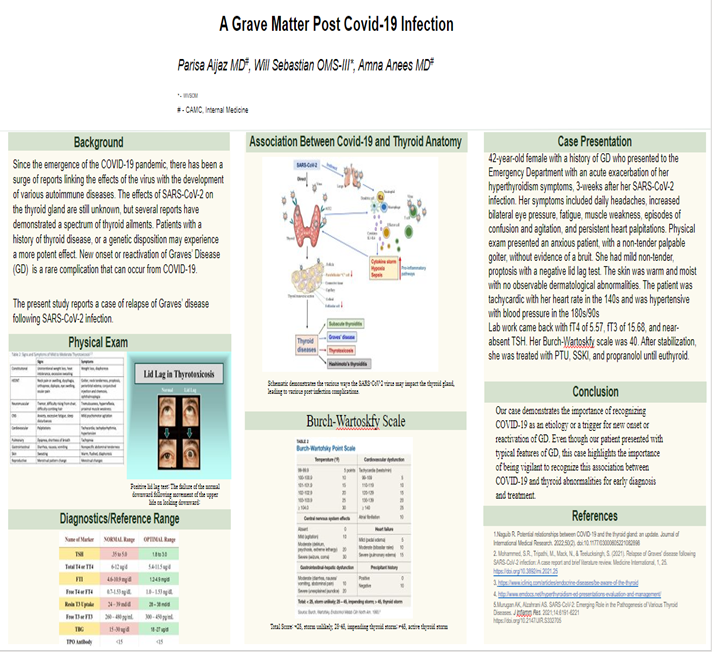
1:10 pm Poster #22 – Case
CASE REPORT: Subxiphoid Pericardial Fluid Collection after Pericardial Window,
Chest Compressions, and Severe Cough
Chloe Kellum – Medical Student - WVU
Preceptor: Shawn Chillag, MD
Pericardial effusion (PE) is an occasional life-threatening problem. Pericardial window is the preferred procedure when effusion recurrence is possible. Surgical access is by either the subxiphoid or trans-pleural approach. Complications are reduced with ultrasound and CT assisted pericardiocentesis but may include cardiac perforation, hemodynamic instability, pericardial decompression syndrome, cardiac arrhythmias, and iatrogenic injury. A case of a 52-year-old man with severe heart failure with reduced ejection fraction and a previously unreported complication is discussed. He presented with complaints of dyspnea and orthopnea for one week with left and right heart failure. Echocardiogram showed an ejection fraction of 15-20% and a moderate posterior PE unamenable to needle drainage, thus a subxiphoid pericardial window was undertaken. During extubation, he went into asystole and was resuscitated with cardiopulmonary resuscitation including chest compressions. An underlying 2-1 atrioventricular block was noted and a dual chamber implantable cardioverter defibrillator was placed. He remained stable and was discharged home. He presented two months later with sharp subxiphoid pain and bulging around the healed incision in the prior 3 weeks made worse with coughing. Chest CT showed a small PE with fluid extension to the subxiphoid soft tissue and bulging with inspiration, Valsalva or cough. Exploration in the operating room found a complete dehiscence of the subcutaneous tissue. The wound layers were reclosed successfully without further PE complications. This case presents a pericardial window complicated by pericardial fluid collection to the subxiphoid space. Chest compressions and severe post-surgical cough likely contributed to wound dehiscence and fluid extravasation. No similar complication was found with extensive search of the literature. The image guided era for pericardiocentesis has resulted in a remarkable reduction in lethal needle trauma. Imaging often immediately identifies a serious problem. This case report is a unique perfect storm.
1:10 pm Poster #22 – Case
CASE REPORT: Subxiphoid Pericardial Fluid Collection after Pericardial Window,
Chest Compressions, and Severe Cough
Chloe Kellum – Medical Student - WVU
Preceptor: Shawn Chillag, MD
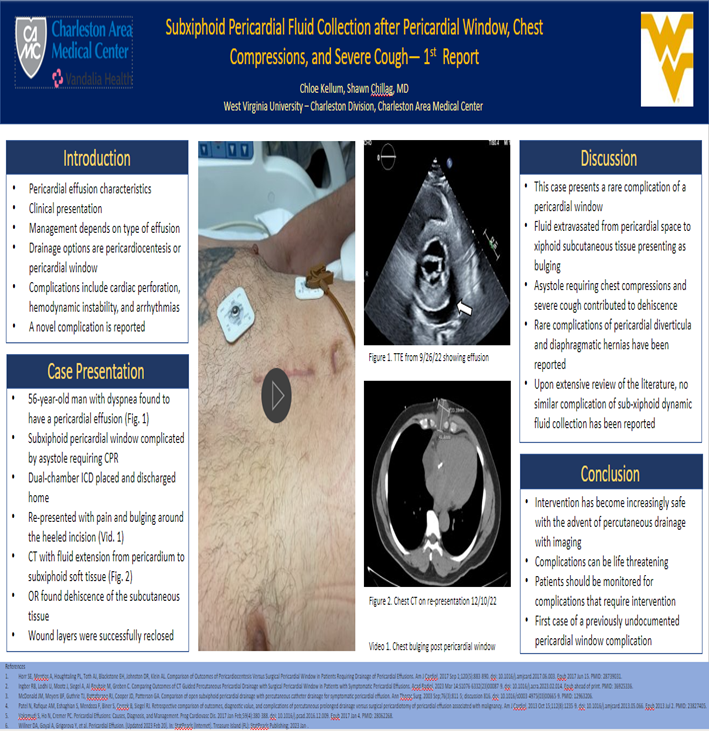
Poster #23 – Case
CASE REPORT: Danger Gummies: Δ8 -THC Induced Psychosis, A Case Series
Manisha Kukkillaya = Medical Student - WVU
Preceptor: James Griffith, MD
Substance induced psychosis is defined in the DSM-5 as delusions and/or hallucinations related to the effects of a substance that cause clinically significant distress or impairment in function. Commonly used substances with a high risk for psychosis include cannabinoids, amphetamines, cocaine, and corticosteroids. Prior studies have suggested a strong link between cannabinoid use and psychosis, proposing that individuals who use higher potency products have an increased risk of developing a psychotic disorder when compared with non-users.
We present a series of 4 patients aged 22 to 50 years-old admitted to the CAMC inpatient psychiatric unit for acute manic episodes after the consumption of delta-8-tetrahydrocannabinol (Δ8 -THC) products in forms of gummies or vape pens. Symptoms included pressured speech, flight of ideas, tangential speech, delusional thinking, poor sleep, and high energy. Two patients had past medical history significant for bipolar disorder, and all endorsed use of Δ8 -THC within one month of symptom onset. Three of the patients used marijuana regularly. One had a prior euphoric episode after ingestion of a Δ8 -THC containing product, while another patient was readmitted for similar symptoms after re-ingesting Δ8 -THC after discharge.
Δ8 -THC is synthetically produced for use in products, unlike the naturally occurring Δ9 -THC. Many factors may contribute to a patient’s progression to mania after use. First, the synthesis of Δ8 -THC-containing products is not regulated by the FDA and thus can result in varying degrees of Δ8 -THC concentrations. Additionally, the endocannabinoid agonist effects of Δ8-THC and
Δ9 -THC have been shown to dysregulate dopamine neurotransmission in animal subjects but not in humans. We hope that this case series encourages physicians to be more familiar with Δ8 -THC products and other potential synthetic cannabinoids that are being introduced to the market, especially with increased use and accessibility.
Poster #23 – Case
CASE REPORT: Danger Gummies: Δ8 -THC Induced Psychosis, A Case Series
Manisha Kukkillaya = Medical Student - WVU
Preceptor: James Griffith, MD
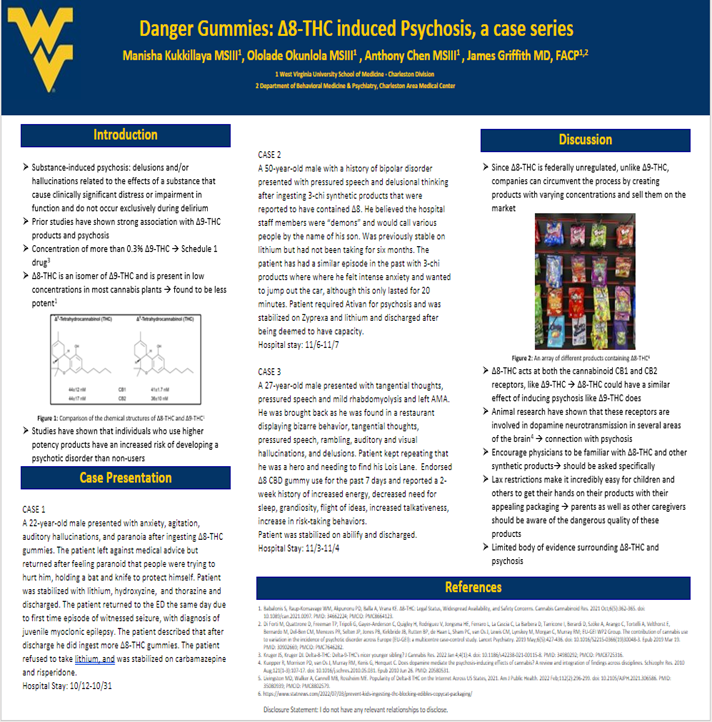
1:30 pm Poster #24– Case
CASE REPORT: All About That Base
Jarrod Kahre, DO – Emergency Medicine
Preceptor: Joshua Burg, DO
Soft Tissue Sarcoma (STS) is a broad term for cancer that originates in soft tissue. This includes cancers developing in muscle, fat, tendons, nerves, lymph, and blood vessels. STS’s are rare, comprising roughly 1% of adult malignancies and 12% of pediatric cancers. There is a large variety of STS’s, each having its own unique characteristics, prognostic indicators, and treatment modalities. Rhabdomyosarcoma (RMS) is the most common tumor in children, and accounts for more than 50% of the cases. RMS forms from skeletal muscle tissue, and can be further classified into subtypes including alveolar, embryonal, and pleomorphic.
A 3-year-old male presented with his mother for left sided gluteal swelling that began 3-4 months ago. The patient was complaining of pain, so she took him to an outlying ED where an Ultrasound was read as “multiple fluid collections, likely hematoma’s.” The pain/swelling slowly improved with symptomatic management, and then worsened once again over the past 6-8 weeks. A CT scan obtained one week ago showed a mass between his left gluteal medius and maximus extending through the sciatic notch into the pelvis. It measured 5.1 x 11.0 x 8.8 cm, causing mass effect on the rectum, surrounding tissues, and possibly the S3 neural foramen. No neurological deficits were noted on examination. Pediatric Oncology admitted the patient with a working diagnosis of sarcoma prior to MRI, biopsy, and staging studies. Surgery indicated the tumor was likely non-resectable at this time and may require neoadjuvant therapy prior to surgical intervention.
Only 400-500 new cases of rhabdomyosarcoma are diagnosed annually in the US, with more than half of those diagnoses occurring in children under 10. Mortality rates have an inverse correlation with age, and children aged 1-9 have the highest survival rate. Prognosis is based on multiple factors including the specific type of RMS, age, origin site, size, and degree of metastasis. Treatment involves a combination of surgery, chemotherapy, and radiation. Few genetic syndromes including NF1, Noonan syndrome, Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, and Costello syndrome have been linked to a higher risk of developing RMS. Interestingly, this patient’s maternal half-sibling was diagnosed with Beckwith-Wiedemann syndrome.
1:30 pm Poster #24– Case
CASE REPORT: All About That Base
Jarrod Kahre, DO – Emergency Medicine
Preceptor: Joshua Burg, DO
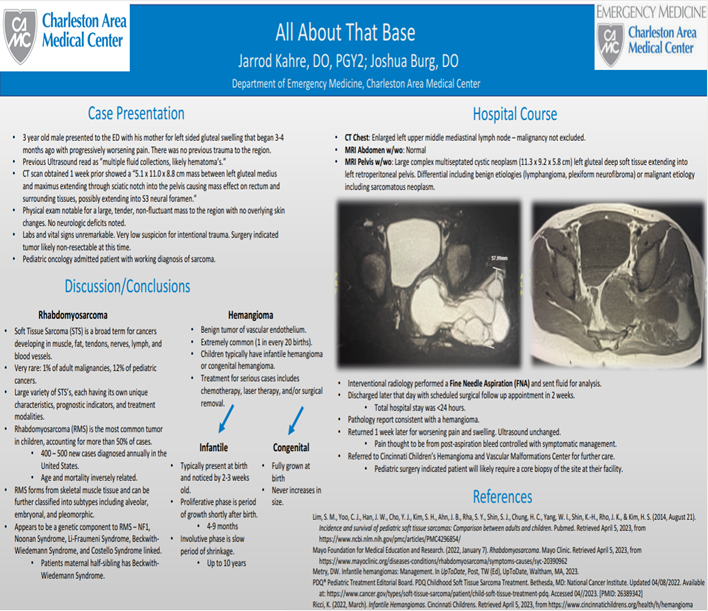
1:50 pm Poster #26 – Case
CASE REPORT: A Case of Severe Neonatal Hypercalcemia Secondary to Subcutaneous
Fat Necrosis Treated with Pamidronate
Zeina Almajthoub, MD- Pediatrics
Preceptor: John Frohna, MD
Introduction
Subcutaneous fat necrosis of the newborn (SCFN) is a rare, self-limiting condition. The pathophysiology is not well understood though complications can occur that may result in significant morbidity and mortality. Identifying these cases and monitoring calcium (Ca+2) levels is necessary.
Case Description
A 20-day-old infant came to the emergency department for evaluation of erythematous, firm subcutaneous nodules on both shoulders, proximal extremities, and buttocks. The baby was born by vaginal delivery at term via a home water birth. Apgar scores were 3, 8, and 10 at 1, 5, and 10 minutes. Skin findings were consistent with SCFN prompting further laboratory studies, which showed: a total Ca+2 level of 15.8 mg/dl (N: 9–11 mg/dl), ionized Ca+2 level 1.77 mmol/l (N: 1.12–1.32 mmol/l), phosphorus 4.7 mg/dl (N: 4.1-9 mg/dl) and 25-OH vitamin D concentration 25 ng/dl (N: 30–100 ng/dl), Ca+2/Creatinine ratio 0.01 (N: <0.82). Despite hyperhydration, calcitonin, and furosemide treatment for 24 hours, Ca+2 only decreased to 13.6 mg/dl. On day 2, an initial dose of pamidronate 0.5 mg/kg was administered. On day 3, due to persistently elevated Ca+2 levels, a 2nd dose of pamidronate was administered. A repeat Ca+2/Creatinine ratio was 0.13. On Day 4, Ca+2 level dropped to 6.8 mg/dl leading to discontinuation of all medications. The baby was observed for 2 days following treatment. A renal ultrasound before discharge showed no evidence of nephrocalcinosis. He was discharged on a low-calcium formula with close follow-up.
Discussion
SCFN is an uncommon condition requiring a heightened level of awareness to secure the diagnosis and manage the complication of hypercalcemia. Intravenous pamidronate is effective at treating hypercalcemia secondary to SCFN. Given pamidronate’s decreased risk of nephrocalcinosis, reduced renal calcium load, and mild side effects compared to furosemide and steroids, it should be considered the first-line treatment in combination with calcitonin and aggressive hydration.
1:50 pm Poster #26 – Case
CASE REPORT: A Case of Severe Neonatal Hypercalcemia Secondary to Subcutaneous
Fat Necrosis Treated with Pamidronate
Zeina Almajthoub, MD- Pediatrics
Preceptor: John Frohna, MD